Case Report

Laparoscopic approach in a case of left paraduodenal hernia
*Ana Margarida Cinza, *Mário Pereira ,*Miguel Rocha Melo, *, Joana Oliveira*Maria Cristina Velez*Rita Lima,*Margarida Amaro, *Jorge Caravana
- *Department of General Surgery at the Hospital do Espírito Santo de ÉvoraLargo do Senhor da Pobreza, 7000-811 Évora, Portugal.
- Submitted:Tuesday, july 28, 2020
- Accepted: Thursday, August 27, 2020
- Published: Sunday, August 30, 2020
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
The Para duodenal hernia represents a herniation of the small intestine in a peritoneal sac found in the fourth portion of the duodenum and it stands as a rare cause for intestinal obstruction.
Case Presentation
The case reports to a 30-year-old male patient diagnosed with a left internal Para duodenal hernia. The patient was admitted for a laparoscopic approach, being submitted to closure of the hernia hole in topography below the Treitz angle. The postoperative period was uneventful.
Conclusions
It is crucial to include Para duodenal hernia in any list of differential diagnosis related to patients with recurrent abdominal pain and occlusive / sub occlusive episodes, in the absence of previous surgeries, abdominal wall hernias or inflammatory bowel disease. When referring to an elective context, the laparoscopic approach is the most appropriate, since it reduces morbidity, postoperative pain and hospitalization time.
Key Words
paraduodenal hernia; minimally invasive surgery; elective surgery
Introduction
Internal hernias are a rare cause of intestinal obstruction (0.2-0.9% of cases of intestinal obstruction and 0.5-4.1% cases of intestinal obstruction caused by hernia)
[2,3]. They are divided into distinct subgroups, based on location, with Para duodenal being the most common type, with a global incidence of 53%
[4].
Para duodenal hernia, also known as congenital mesenteric-parietal hernia, represents a herniation of the small intestine in a peritoneal sac found in the fourth portion of the duodenum. The most frequently found fossae are: lower than Treitz (60%), upper and lower (30%), upper (5%), Landzert Fossa (2%) and Waldeyer Fossa (1%) [1]. On the other hand, there are two types of congenital paraduodenal hernia: left (75%) and right (25%), depending on the anatomical component and embryological involvement. In the right paraduodenal hernia, the hernia contents protrude into the Waldeyer fossa, while in the left paraduodenal hernia, the hernia occurs in the Landzertparaduodenal fossa [6].
The signs and symptoms associated with left paraduodenal hernia are generally nonspecific, with a clinical presentation that can vary from intermittent abdominal pain, linked to the possibility of spontaneously reducing the hernia content, to an acute abdomen, in situations of incarceration and intestinal necrosis
[5].
Case Presentation
The case reports to a 30-year-old male patient with complaints of an insidious illness, characterized by several years of evolution and marked by a profound deterioration within the previous 3 months. The patient reported episodes of constipation alternated with diarrhea, the presence of a feeling of bloating and occasional vomiting, in the absence of weight loss or any other complaints. The patient denied the existence of any relevant personal, surgical, or familiar history. He underwent an abdominal and pelvic computerized tomography which revealed a discontinuous filling of the Jejunal loops after oral administration of a contrast agent, with a hiatus development between the jejunum and the ileum. This finding was compatible with a left internal Para duodenal hernia (Fig 1 2), without an associated disturbance of the gastrointestinal transit or abnormality of the morphology of the intestinal loops. Additionally, sthe patient was submitted to a colonoscopy and analytical evaluation including measurement of tumor markers. A thorough study of the intestinal transit was also performed, through the administration of an oral contrast agent. These investigations resulted unremarkable.
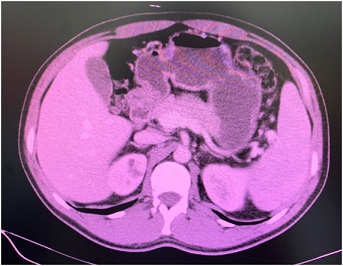

Figure 1: Oral discontinuous contrast showing left paraduodenal hernia

Figure 2: Appearance of left paraduodenal hernia on CT scan
In this context, a diagnostic laparoscopy was performed, the hernia content was reduced and the hernia hole in topography below the Treitz angle closed with silk (Fig 3 , 4 5, 6).

Figure 3: Patient positioning and trocars placement

Figure 4: Treitz Angle and exposure of the hernial hole

Figure 5: Closure of hernial hole with silk

Figure 6: Appearance of hernial hole closed
The immediate postoperative recovery was uneventful, and the patient was discharged on the second postoperative day, with intestinal transit restored. At follow-up, and nineteen months post surgery, he remained asymptomatic.
Discussion
Paraduodenal hernia is a rare cause of intestinal obstruction that should be considered in any patient with recurrent abdominal pain, bowel obstruction, without history of previous surgery, abdominal wall hernias or inflammatory bowel disease [1, 4].
The most likely pathophysiological mechanism for the existence of left paraduodenal hernias is linked to embryological anomalies, particularly related to a poor rotation of the intestine during the first weeks of pregnancy [5, 6].
From a diagnostic point of view, neither simple abdominal radiographs nor abdominal ultrasound examination are useful. Thus, in the presence of a left paraduodenal hernia, the use of abdominal computed tomography is the gold standard for diagnosis, making possible to detect the encapsulation of the bowel loops with intermittent dilation, either at the level of the Treitz ligament or above [3].
The treatment of Para duodenal hernia is surgical and lies in two main principles - reduction of hernia content, in which excision of the hernia sac is not mandatory, and correction of the hernia orifice, through its closure or enlargement; it may be necessary to distort the involved intestine, in order to avoid lesions in the main mesenteric vessels contiguous to the hernia orifice [3, 4, 6].
The laparoscopic approach offers several advantages, since it is safe, results in less morbidity, reduces postoperative pain, promoting earlier enteric diet introduction and a shorter hospital stay with a greater aesthetic satisfaction
[1].
Conclusions
Summing it all up, an early diagnosis of Paraduodenal hernia is essential. A relatively high degree of clinical suspicion is important in order to avoid the establishment of an occlusive condition and intestinal strangulation. Abdominal computed tomography is the gold standard for diagnosis. The laparoscopic approach is adequate and frequently elected to achieve surgical resolution of this pathology, once it can be performed safely and is associated with very satisfactory results for the patient. The authors were able to understand the need and importance of an early diagnosis in cases of intestinal occlusion due to rare causes, such as internal Para duodenal hernias, and to establish the advantages of a laparoscopic approach to achieve surgical treatment of the condition. This particular case highlighted and corroborated the excellent results that had already been obtained in other hospitals using this technique.
Authors' Contribution
AMC: responsible for patient’s investigation, outcome and
follow-up; participation on patient’s surgery; conception, design and
composition of the manuscript guided by the actual data and evidence; critical
revision.
MP, MRM, JO, MCV, RL: responsible for patient’s
investigation, diagnosis, patient’s surgery, outcome and follow-up, data
analysis, interpretation and also for doing the critical revision of the
article; approved the final version to be published.
MA: important contributions to the Conception and design of
the manuscript, drafting the article and doing critical revision; approved the
final version to be published.
JC: important part of clinical and treatment judgment by
multidisciplinary evaluation, made critical revision of the article and approved
the final version to be published.
All people who meet authorship criteria are listed as
authors, and all authors certify that they have participated sufficiently in the
work to take public responsibility for the content, including participation in
the concept, design, analysis, writing or revision of the manuscript.
Conflicts of interest
We have no conflict of interest to declare.
Funding sources
The authors have no funding source to disclose for this work.
Ethical approval
The submitted article is a case report, ethical approval has beenexempted by our institution.
Consent
Written informed consent was obtained from the patient forpublication of this case report and accompanying images.
Copy of consent is available with authors.
References
[1]. Wakabayashi M, Kono S, Takahashi T.
Laparoscopic repair of acute small bowel obstruction due to left paraduodenal
hernia: A case report. Int J Surg Case Rep. 2018;51:194-199. [PubMed] [PMC full Text]
[2]. Manipadam JM, V L, Syamprasad V, H R.
Laparoscopic Repair of a Right Paraduodenal Hernia. Surg J (N Y). 2018 Jul
20;4(3):e129-e132 [PubMed] [PMC Full Text]
[3]. Takagishi T, Niimi Y, Matsuki G,
Nagano S, Hinami J, Kajiwara M, Kaneko K, Kubota Y, Nakai O. Laparoscopic Repair
of Right Paraduodenal Hernia in Adult Patients: Case Report and Literature
Review. Case Rep Surg. 2018 Oct 15; 2018: 9691689. [PubMed][PMC Full text]
[4]. Correia M, Amonkar D, Audi P, Vaz O,
Samant D.; Paraduodenal hernia: A case report and review ofthe literature. Saudi
Surgical Journal 2014;2:96-8 [Full
Text]
[5]. Shadhu K, Ramlagun D, Ping X.
Para-duodenal hernia: a report of five cases and review of literature. BMC Surg.
2018 May 30;18(1):32 [PubMed] [PMC Full Text]
[6]. Mehra R, Pujahari AK. Right
paraduodenal hernia: report of two cases and review of literature. Gastroenterol
Rep (Oxf). 2016 May;4(2):168-71
[PubMed] [PMC Full text
[7]. Sleiman Y, El-Kheir A, El-Khoury M,
Hamdach O, Ismail L, Allouch M. Small bowel obstruction secondary to left
paraduodenal hernia: A case report and literature review. Int J Surg Case Rep.
2018;53:29-31 .[Pubmed] [PMC Full Text]

