Case Report

Osteomyelitis as a Rare Complication of Laparoscopic Cholecystectomy: A Case Report
1N.A.G. Hakkenbrak, 1 L.S. Boogerd, 1D.E. Moes,1L.M. de Brauw
- 1.1Department of Metabolic and Bariatric Surgery, MC Slotervaart, Amsterdam, the Netherlands.
- Submitted Thursday, September 19, 2019;;
- Accepted Thursday, October 24, 2019;
- Published Wednesday, October 30, 2019
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction:
Laparoscopic cholecystectomy is one of the most commonly performed surgical procedures worldwide. A small percentage of patients revisit the hospital or outpatient clinic with post-operative complications such as infection, bleeding, biliaryor bowel injury. In this case report, we describe a very rare complication.
Case Presentation:
A 71-year-old male presented at our outpatient clinic with abdominal pain and fatigue. The patient had been admitted abroad, two months before, with biliary pancreatitis and cholangitis due to choledocholithiasis for which laparoscopic cholecystectomy was performed. However, the abdominal pain increased. Additional imaging showed intra-abdominal abscesses. After one month of treatment the patient visited the emergency room with a painful swelling of the right lower thoracic cavity. Follow up CT-scan showed reduction of the sub-hepatic abscess but swelling surrounding the 11thrib suggestive of osteomyelitis. Therefore, the patient was operated and the rib was partially resected. Intravenous antibiotics were continued based on tissue cultures.
Conclusion:
An intra- abdominal abscess is a rare complication after laparoscopic cholecystectomy (<1%). Spillage of stones or bile increases the risk of abdominal abscesses. In this case report the sub-hepatic abscess migrated towards the rib resulting in osteomyelitis. Given the therapeutic difficulty of osteomyelitis, aggressive treatment is necessary to prevent this complication and limit further harm.
Keywords:
bile stones, bile spillage, postoperative complication.
Introduction
Cholecystectomy is one of the most commonly performed surgical procedures worldwide [1]. Serious post-operative complications have been described in 2.6% of the patient population [2]. These include bleeding, intra-abdominal abscess, bile leakage, biliary -and bowel injury [2]. In this case report we describe the very rare case of osteomyelitis of the rib after laparoscopic cholecystectomy.
Case Presentations
A 71-year-old male presented to our outpatient clinic with abdominal pain. Two months before presentation the patient had been admitted to a hospital in Spain with biliary pancreatitis and cholangitis due to choledocholithiasis. Initially, an endoscopic retrograde cholangiopancreatography (ERCP) with papillotomy and percutaneous drainage of the gallbladder was performed.
Laparoscopic cholecystectomy was executed in the same admission. During surgery the gallbladder appeared to be perforated causing spillage of bile and stones. Therefore, an abdominal drain was placed and additional doses of antibiotics were given after surgery. Previous medical history revealed coronary ischemia and Brugada syndrome for which an implantable cardioverter defibrillator had been placed and partially removed due to inactivity.
Back in the Netherlands the patient visited our outpatient clinic with fatigue and persistent abdominal pain without nausea or vomiting. During physical examination there were no signs of systemic infection like fever or tachycardia. Normal bowel movements and tympani were observed, but palpation of the right upper abdomen was very painful. Laboratory findings showed slightly elevated liver enzymes with normal inflammation parameters [Table 1]. A computed tomography-scan (CT-scan) was performed, two small abscesses were seen; a subhepatic abscess measuring 24x48x16 mm (located near liver segment 6 and towards the paracolic gutter) and a second abscess in Douglas measuring 30x20x16 mm (Figures 1).
Table 1: Reported cases of epidermoid cyst of the cecum in the literature.
| |
Presentation |
+ 2 weeks |
1st admission |
2nd admission |
Reference |
| CRP |
8.4 |
73 |
42 |
23 |
<10 mg/l |
| Leukocytes |
9.2 |
10 |
8.4 |
8.1 |
4.0-10.0 x 109/l |
| AF |
169 |
125 |
|
|
<125 U/l |
| gGT |
144 |
46 |
|
|
<45 U/l |
| ALAT |
40 |
15 |
|
|
<50 U/l |
| ASAT |
24 |
16 |
|
|
<45 U/l |
| Bilirubine |
27 |
24 |
|
|
<17 µmol/l |
| Lipase |
52 |
25 |
|
|
20-140 U/l |
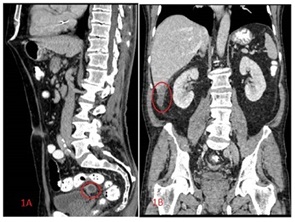

Figure 1. Intra- abdominal abscess: A. sub-hepatic abscess, near segment 6 of the liver. B. Abscess in Douglas.
During the following month, the abdominal pain increased and migrated towards the right thoracic cavity. The inflammation parameters were slightly elevated without clinical signs of a systemic infection (Table 1). Ultrasonography and a CT-scan showed reduction of the sub-hepatic abscess, the abscess in Douglas was not retrieved on CT-scan (Figure 2). The abscess was drained and antibiotic treatment was started (amoxicillin/clavulanate 500/125mg p.o. 3dd1 tablet).

Figure 2. Follow up CT scan: One month after presentation showed reduction of (A) the sub-hepatic abscess (10 x 34 x 7 mm) and (B) no signs of abscess in Douglas.
One week later the patient visited the emergency room because of unbearable pain without fever or tachycardia. A painful swelling of the right lower thoracic cavity without redness of the skin was seen during physical examination. Ultrasonography showed migration of the hepatic abscess to the lateral abdominal wall, 14 mm underneath the skin. Patient was admitted to the hospital and treated with intravenous Ceftazidime (3dd 2000mg) based on tissue cultures. The CT-scan showed reduction of the sub-hepatic abscess and swelling surrounding the 11th rib. After one week, the pain decreased and the patient was discharged.
However, despite treatment, two months after the first hospital admission, the patient was readmitted to the hospital because of unbearable pain. CT-scan was repeated and showed soft tissue swelling towards the 11th rib, suspected for osteomyelitis (Figure 3). During surgery the abscess and osteomyelitis of the 11th rib were seen. Hence, the rib was partially resected, debrided and a gentamycin coated patch was placed in the wound. The patient received negative pressure therapy for the wound and intravenous Ceftazidimefor six weeks. Three and a half months after surgery the wound was completely healed and the pain disappeared.

Figure 3. CT-scan: (A-B) Soft tissue infection with direct contact of the 11th rib, suggestive of osteomyelitis. No signs of abdominal abscesses.
Discussion
Abdominal Abscess
In approximately 35% of laparoscopic cholecystectomies spillage of bile and gallstone(s) occur due to gallbladder perforation [3]. In 0.6% abscesses develop after bile spillage compared to 0.6-2.9% after both bile and gallstone spillage [3]. Spilled stones or fragments can migrate anywhere in the abdominal cavity and can result in arrange of complications e.g. abscesses (mostly located in the abdominal wall or abdominal cavity: sub-hepatic space or retroperitoneum) or fistulae (ranging from fistulas of the skin to colovesical fistulas) [3-5]. Stone retrieval, abscess evacuation or flushing of the abdominal cavity has been described to be successful after stone spillage during surgery [6]. However, in case of intra-abdominal abscess, percutaneous drainage and antibiotic treatment based on tissue cultures is adviced [6].The described mean duration for the development of abscesses after laparoscopic cholecystectomy range from 4 months up to 10 years [7].
Pseudomonas
Abscesses due to Pseudomonas have been described as complication of laparoscopic cholecystectomy due to their location as commensal- bacteria in the biliary system [8]. Organisms found in bile cultures regard Escherichia coli (75%), Klebsiella (19%), Pseudomonas (3%) and circa 3% gram negative rods (species non specified) [8].Pseudomonas aeruginosa is a gram-negative aerobic bacillus and associated abscesses are best treated with local surgical excision and antibiotics for a period of 6 weeks [9]. Studies on Pseudomonas osteomyelitis are limited and contain heterogeneous data due to the rarity of the infection. The disease remains a therapeutic challenge and is often associated with a high rate of relapse [9].
In conclusion, this case report describes a patient who developed abscesses and osteomyelitis of the rib after bile- and stone spillage during laparoscopic cholecystectomy. Taken into account that intra-abdominal abscesses are a rare complication, osteomyelitis due to these abscesses was not primarily considered. Therefore, imaging should be performed in case of persistent abdominal or skeletal pain after laparoscopic cholecystectomy. Aggressive treatment is necessary to prevent complications and limit further given the therapeutic difficulty of osteomyelitis.
Learning Points
1.Laparoscopic cholecystectomy is one of the most common performed surgical procedures with approximately 2.6 % serious postoperative complications including bleeding, abscess, bowel- and biliary injury.
2.The majority of abdominal abscesses occur after spillage of bile or stone fragments, mostly located in the abdominal wall, sub-hepatic or retroperitoneum.
3.Pseudomonas aeruginosa is a common micro-organism in bile and requires aggressive treatment in case of related complication.
Declarations
Consent of patient written informed consent was obtained from the patient for publication of clinical details and imaging.
Conflict of Interest
The authors declare that they have no competing interests regarding the publication of this paper.
Authors’ Contributions
All authors participated in the writing and revision of the manuscript.
NH selected patient data and was responsible for conception and writing of the manuscript. LB reviewed the selected data and responsible for completing the manuscript. DM and LM reviewed and revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
None
References
[1].Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180(1):101-25.[PubMed]
[2].Thurley PD, Dhingsa R. Laparoscopic cholecystectomy: postoperative imaging. AJR Am J Roentgenol. 2008;191(3):794.[PubMed]
[3].Ji Yeon Kim, Kyoung Won Kim, Chul-Soo Ahn, Shin Hwang, Young-Joo Lee, Yong Moon Shin and Moon-Gyu Lee. Spectrum of biliary and nonbiliary complications after laparoscopic cholecystectomy: radiologic findings. American Journal of Roentgenology. 2008; 191:783-789.[Pubmed]
[4].Woodfield JC, Rodgers M, Windsor JA.Peritoneal gallstones following laparoscopic cholecystectomy: incidence, complications, and management. Surg Endoscopy. 2004;18:1200–1207.[Pubmed]
[5].Zehetner J, Shamiyeh A, Wayand W. Lost gallstones in laparoscopic cholecystectomy: all possible complications. Am J Surg. 2007; 193:73-8.[Pubmed]
[6].Shamiyey A, Wayand W. Laparoscopic cholecystectomy: early and late complications and their treatment. Langenbecks Archives of Surgery. 2004;389 (3)164–171.[Pubmed]
[7].Khalid M, Rashid M. Gallstone abscess: a delayed complication of spilled gallstone after laparoscopic cholecystectomy. Emergency Radiology.2009; 16(3)227–229[PubMed]
[8].Jain N, Neogi S, Bali RS, Harsh N. Relationship of Gallbladder Perforation and Bacteriobilia with Occurrence of Surgical Site Infections following Laparoscopic Cholecystectomy.Minimally Invasive Surgery. 2015;204508.[Pubmed] [PMC Full text]
[9].N. Laghmouche, F. Compain, AS Jannot, P Guigui, JL. Mainardi, G. Lonjon, B. Bouyer, MP Fernandez-Gerlinerg. Successful treatment of Pseudomonas aeruginosa osteomyelitis with antibiotic monotherapy of limited duration. Journal of infection.2017; 75(3):198-206[PubMed]

