Case Report

Giant Cell Arteritis – A Medical Emergency in Elderly
* Miguel Ricardo, * Ana Oliveira, * Célia Cruz, * Tânia Ferreira, * Filipa Silva
- * Department of Internal Medicine, Centro Hospitalar do Porto – Hospital de Santo António, Porto, Portugal
- Submitted: Monday, November 21, 2016
- Accepted: Monday, December 26, 2016
- Published: Thursday, January 5, 2017
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Giant Cell Arteritis is the most frequent vasculitis in elderly and represents a potentially reversible cause of blindness in this population. The prognosis depends on how quickly the therapy is initiated, that is why a high index of suspicion is important to the diagnosis, allowing the immediate initiation of appropriate treatment. We present a typical case of Giant Cell Arteritis in a patient who arrived four days after the onset of symptoms in the emergency room. The delay in presentation may have dictated his prognosis despite prompt onset of corticosteroid therapy.
Keywords
Giant Cell Arteritis, Temporal Arteritis, Anterior Ischemic Optic Neuropathy
Introduction
Giant Cell Arteritis (GCA), or Temporal Arteritis, is the most common vasculitis in elderly, [1] its incidence can rise to 27 cases per 100.000 persons older than 50 years, being the mean presentation age 70 years [2]. It’s characterized by granulomatous inflammation of medium and large arteries, [1- 3] with predilection for extracranial branches of carotid and vertebral arteries [3,4].
Classical presentation includes new onset headache and constitutional symptoms, with or without jaw claudication [3]. Visual loss happens in at least 70% of the cases and is the biggest cause of morbidity, [4] occurring alone in up to 20% of the patients [2,4,5]. It’s the result of the occlusion of the vessels of the eye, optical disk or brain parenchyma [6]. The most common cause is anterior ischemic optic neuropathy (AION), [2,4] which manifests by sudden and painless loss of vision or loss of a visual field, [4] irreversible in 15 to 20% of the cases, [1,2] even with proper treatment. However, involvement of the contralateral eye, that happens within days to weeks in 60% of the patients, [2-4] can be avoid if the vasculitis is readily treated [7].
Laboratory findings are related with the presence of an active inflammatory state. The sedimentation velocity (SV) and reactive C protein (RCP), although don’t be specific, are very sensitive, especially when above 90mm/h and 90mg/L, respectively, [4], however the absence of raise don’t exclude the diagnosis [3]. Temporal artery biopsy remains the gold standard for the GCA diagnosis, [2, and 4] identifying 85-95% of the cases [6] Moreover, has a prognostic value, since a positive result tightly predicts neuro-ophthalmologic complications [3].
Systemic corticotherapy is the basis of GCA treatment, and shouldn’t be delayed by the biopsy result [2], especially when there is ocular involvement [1, 3, and 6]. The presence of eye achievement is formal indication for corticosteroid bolus (1000mg/day) for the first three days, followed by 1mg/kg/day oral corticoid (maximum 60mg/day), recommended ad initium for the remaining patients with GCA [4,6]. This dose shall be continued until the resolution of the symptoms and the normalization of the inflammatory parameters, being then, slowly reduced over several months [5,6]. In most patients, systemic inflammatory symptoms and signs rapidly responds to the high corticoid dose, [6] in contrast with visual changes that are usually irreversible [1, 4].
Case Report
79 years-old man, with arterial hypertension, type 2 diabetes mellitus (DM) and dyslipidemia, presented to the emergency department with loss of left lower visual field, neck pain, bilateral temporal and frontal headache and scalp tenderness, with a poor response to ibuprofen, since last four days. There was no history of previous similar complaints, constitutional syndrome, jaw claudication or pain/weakness at the shoulder or hip girdle.On examination, he presented with a blood pressure of 211/116mmHg, heart rate of 86 beats per minute, apyretic and with peripheral oxygen saturation of 98%. His temporal pulse was weak, no painful to palpation, and he had a severe loss of visual acuity of the lower fields of the left eye. The funduscopic examination revealed a pallid and swollen optic disk with superior temporal exudates.
Laboratorial findings included normocytic normochromic anemia, low total iron- binding capacity and high ferritin, reactive C protein (RCP) 91mg/L (reference range 0-5mg/L) and sedimentation velocity (SV) 93mm/h (reference range 0-30mm/h). Syphilis, brucellosis, B and C hepatitis, human immunodeficiency virus, Epstein-Barr virus, herpes simplex virus and parvovirus serologies were negative. Cranioencephalic computerized tomography (CT) angiogram scan didn’t show acute ischemic or hemorrhagic lesions, vascular dissections, aneurysmal formations or arteriovenous malformations.
Assuming giant cell arteritis as the most likely diagnosis, it has been initiated immunosuppressive therapy with systemic corticotherapy. Still on the first day of treatment, was performed a left temporal artery biopsy, with the acquisition of a sample of 18x3mm. This confirmed, a posteriori, the diagnosis, revealing an inflammatory infiltrate of the arterial wall and multinucleated giant cells (Figure 1).
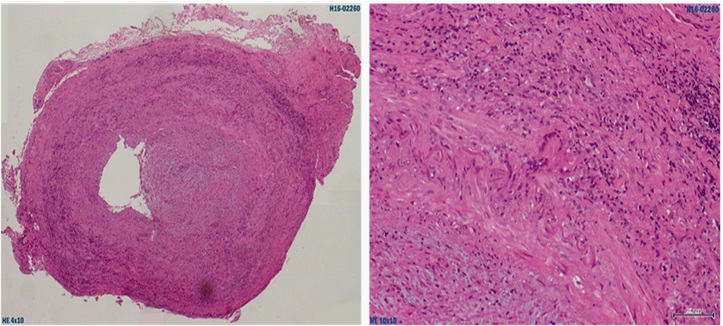
Figure 1: Left temporal artery biopsy, with typical histological findings of GCA. On the left side, cross section (HE, 40x), with diffuse inflammatory infiltrate of the arterial wall. On the right, in detail (HE, 100x), a multinucleated giant cell, typical of this disease.
Despite the early institution of proper treatment, the visual acuity of the left eye remained unchanged. On the other side, there was no recurrence of headache and the right eye visual acuity was not affected. The SV dropped to 57mm/h and the RCP became normal. A thoracic aortic aneurism was excluded.
During the hospitalization, there were no side effects of the corticotherapy, except for the decompensation of DM, requiring the introduction of insulin therapy. He was discharged medicated with prednisolone, acetylsalicylic acid, insulin, metformin, calcium and vitamin D and bisphosphonate. Patient was also started cotrimoxazole to prevent Pneumocystis carinii infection.
Three months later, at the consultation, under 10mg of prednisolone per day, he presented with no changes in the visual acuity, without recurrence of the headache or any other signs or symptoms. RCP was 2.47mg/L and VS 31mm/h.
Discussion
When any elderly presents with ophthalmologic complaints, the hypothesis of a GCA must be always considered, which will allow reducing the risk of permanent visual loss. In the presented case, the age of the patient and the loss of visual acuity raised immediately the provisional diagnosis of a GCA. There were, however, some facts that could have reduced the index of suspicion. Firstly, this entity develops predominantly in women, [2] with a ratio man/women of 1:3 [1,7]. Furthermore, the vascular risk factors that our patient presents and the values of blood pressure that he presented on the emergency department could raise de hypothesis of a hypertensive emergency with ocular involvement.
The headache, usually bitemporal, is the most common symptom [2-4]Specific symptoms include jaw claudication (the most specific), [2,4] scalp tenderness and pain, knotty swelling or diminished pulse of the temporal artery [1,3,4] Between these, our patient presented with scalp tenderness and weakness of left temporal pulse, contributing to the diagnostic. Since this is an inflammatory disease, until a third of the patients can present with constitutional symptoms as fever, night sweats, fatigue, anorexia and weight loss [1, 3,and 4]. It has been excluded symptoms and signs of Polymyalgia Rheumatica (PR), once in about 50% of the cases the GCA is associated with this entity [1, 2, 4, and 7]. On the other side, only 5-15% of the patients with PR will be diagnosed with GCA [1, 2].
While the visual loss pattern, altitudinal (horizontally limited), presented by our patient is more characteristic of non-arteritic causes of AION, the funduscopic exam was highly suggestive of an arteritic cause, usually characterized by swollen and pale optic disk, and, eventually, hemorrhages, exudates and cotton-wool spots in the retina [2-4].
Regarding the laboratory findings, and consistently with the physiopathological basis of the disease, besides the rise in RCP an SV, our patient presented also normocytic normochromic anemia, leukocytosis, thrombocytosis and low serum albumin, which are usual findings [2-4]
Definitive diagnosis had been confirmed by the findings in the temporal artery biopsy, performed, accordingly with the recommended by the literature, at the most symptomatic side and with an extension of at least 15 to 30mm, because of the typical discontinuous arterial involvement (skip lesions), which can lead to false negative results [2, 3, 5]. The fact that the biopsy was performed at the first day of treatment with corticosteroids also decreased the likelihood of a false negative result that is more frequent after the second week of immunosuppressive treatment [2-4]. Typical findings include diffuse infiltrate of mononuclear cells of the arterial wall, intimal proliferation, fragmentation of the internal elastic lamina and the presence of macrophages and multinucleated giant cells [4 5].
Since there is previous description of ischemic complications related to the development of aneurisms and stenosis of big (in until 83% of the cases) and cranial vessels, [1, 2, 4, 8] those were actively searched with cranioencephalic and thoracic CT angiogram, that didn’t revealed any alterations. Also the coronary or mesenteric arteries can be involved, resulting in local ischemic complications [4]. Universal use of a low dose (75-150mg/day) of acetylsalicylic acid is controversial, [6] but some studies suggested that it can reduce the risk of visual loss and other intracranial ischemic complications [3-5].
The visual alterations weren’t, unfortunately, reverted, despite the quick onset of treatment, which was not a surprise, since the patient only came to the emergency department four days after the beginning of the visual loss. This highlights the fact that GCA is a real medical emergency. Nevertheless, the involvement of the other eye may have been spared thanks to the treatment.
Weaning from corticosteroids is difficult and can be associated with relapses with new onset polymyalgia, ischemic complications or AION recurrence, [2 ,6] which usually respond to an increase in the corticosteroid dose but can, in some cases, require ad eternum medication [4,6]. Although their importance in the patient’s monitoring, an asymptomatic raise in RCP or SV should not motivate therapeutic changes [6].
Up to 86% of the patients can suffer adverse effects of corticotherapy, so, it’s important to individually evaluate the necessary measures to its prevention or reduction. In some cases can even be necessary to try the introduction of corticoid sparing agents, as methotrexate or azathioprine [1 4].
The risk of recurrence, ischemic complications and iatrogenic effects isn’t negligible, requiring a close and long-term monitoring of these patients.
Learning points
When an elderly presents with visual loss, giant cell arteritis must always be considered.
Treatment with systemic high dose corticotherapy may not recover the visual acuity lost, but can prevent the contralateral eye involvement.
Close and long term monitoring is important, due to potential complications not only of the disease but also of the treatment.
Authors’ contributions
MR: searched data and edited the manuscript
AO: critically reviewed and helped in final version of the manuscript CC: critically
reviewed and helped in final version of the manuscript TF: helped in data research and manuscript redaction
FS: helped in data research and manuscript redaction
Conflict of interests
There are no conflict of interests.
Ethical considerations
The written consent was obtained from the patient for publication of this case report.
Funding
There were no fundings.
References
[1]. Kesten F, Aschwanden M, Gubser P, Glatz K, Daikeler T, Hess C. Giant cell arteritiis – a changing entity. Swiss Medical Weekly. 2011; 141: w1327 [Pubmed]
[2]. Chacko JG, Chako JA, Salter MW. Review of Giant cell arteritis. Saudi Journal of Ophthalmology. 2015; 29: 48–52.[Pubmed]
[3]. Caylor TL, Perkins A. Management of Polymyalgia Rheumatica and Giant Cell Arteritis. American Family Physician. 2013; 88(10): 676-684. [Pubmed]
[4]. Ness T, Bley T, Schmidt W, Lamprecht P. The Diagnosis and Treatment of Giant Cell Arteritis. Deutsches Ärzteblatt International. 2013; 110(21): 376−86 [Pubmed]
[5]. Zwicker J, Atkins EJ, Lum C, Sharma M. An atypical presentation of giant cell arteritis. CMAJ. 2 de Março de 2011; 183(5): E301-E305.[Pubmed]
[6]. Weyand CM, Goronzy JJ. Giant-Cell Arteritis and Polymyalgia Rheumatica. N Engl J Med. 2014; 371(1): 50–57 [Pubmed]
[7].Weyand CM, Liao YJ, Goronzy JJ. The Immunopathology of Giant Cell Arteritis: Diagnostic and Therapeutic Implications. J Neuroophthalmol. 2012; 32(3): 259–265 [Pubmed]

