Case Report

A Case of Wristwatch Ingestion in a 7 Year Old
2Sarita Chowdhary, 1Dinesh Kumar, 2 Mohd Zeeshan Hakim., Shiv Prasad Sharma
- Departments of 1Paediatric Surgery and 2General Surgery, Institute of Medical Scinces, Banaras Hindu University, Varanasi, India
- Submitted: Thursday, July 14, 2016
- Accepted: Friday, August 19, 2016
- Published: Friday, November 25, 2016
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Ingestion of foreign objects is very common in children and must be dealt with caution. Early intervention can be avoided by serial monitoring. The case of ingesting an entire wrist watch is scarce, although smaller button batteries and coins do top the list. Careful assessment and proper decision making to the time of surgery is crucial for appropriate management.
Key Words
Foreign Body, Paediatric patients, plain x-ray, endoscopy.
Introduction
Foreign body ingestion is not uncommon in children, it was reported that more than 125,000 patients in the age group 19 years or less presented to the emergency department in the US in 2007 [1]. A recent study carried out in the US between 2002 and 2011 found 16386 children presenting to the emergency department with possible magnet ingestion, with an 8.5 fold increase in incidence between 2002 and 2011; majority of these patients were below 5 years of age [2].
Ingested fish bones have been one of the most common foreign bodies found among the areas where fish is a major dietary contributor. The peak incidence is between 6 months and 6years and is nearly equal among both sexes [3, 4, 5, 6]. Most foreign bodies that are small tend to pass harmlessly through the GIT. Impactions, obstructions and perforations occur at GI angulations and narrowing. Thus, children with congenital malrotations or who have undergone GI surgery have greater risk of obstruction and perforation. Identification of the area of impaction is often vague, although, the presence of frank oesophageal perforation in the form of neck swelling, erythema, tenderness, crepitus can be a useful guide. Abdominal signs in the form of guarding and rigidity preclude emergent laparotomy. Biplane radiographs can identify most foreign bodies and free mediastinal or peritoneal air.
Case Report
A 7 year old male child presented with history of ingestion of a wrist watch one week back, which was observed by his grandfather. He presented with no difficulty in deglutition and had no signs of an acute abdomen; however, he had not passed the watch in his stools till date. Plain radiographs revealed the presence of the wrist watch in the abdomen (Figure 1).

Figure 1: Plain radiograph of Abdomen at presentation (after 1week of ingestion), showing the watch in the upper abdomen
The child was kept on soft diet for 48 hours and serial radiograph revealed little change in position of the object. Elective laparotomy was considered for the child. Upon laparotomy, the watch was recovered from the stomach at the antro-pyloric junction. The child recovered uneventfully in the post-operative period and was discharged after 5 days of the procedure (Figure 2,&3),
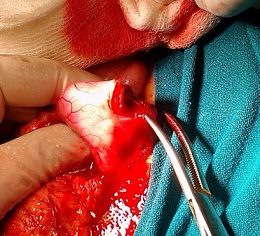
Figure 2: The watch discovered in the gastric antrum on laparotomy
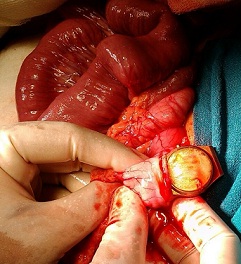
Figure 3: The watch retrieved on Gastrotomy
Discussion
The ingestion of foreign body is one of the most common complications as a result of the oro-exploratory behaviour in small children. As note earlier, the maximum incidence is noted in the 6month to 6year age group. The case discussed here reveals the operative intervention performed for a wrist watch, an inch long foreign object, which the child ingested a week earlier, the object, was noted in the upper abdomen and exploratory laparotomy was done. Foreign body ingestion is usually harmless if the ingested foreign body is small or blunt (smaller than 2.5cm is considered harmless) [7, 8], however, for long (>6cm) or sharp, the management protocols call for a more active monitoring. Patients suspected of swallowing sharp-pointed objects must be evaluated to define the location of the object. Many sharp-pointed objects are not radiographically visible, so endoscopy should still follow a radiologic examination with negative findings. Direct laryngoscopy is often used to remove objects lodged at or above the cricopharyngeal sphincter. Otherwise, rigid or flexible endoscopy may be performed when laryngoscopy is unsuccessful or for treatment of objects lodged below this area
[9]. Most of the sharp-pointed objects that reach the stomach pass without incidence; the risk of a complication caused by a sharp-pointed object can be as high as 35% [10]. Therefore, a sharp-pointed object that has passed into the stomach or proximal duodenum should be retrieved endoscopically if this can be accomplished safely [11, 12]. Long objects on the other hand have difficulty in passing through the duodenum and hence, retrieval through endoscopic means is essential. Concern regarding ingestion of disk or button batteries and magnets that are harmful to the body and risk perforation is increased if the battery gets lodged into the oesophagus or any other part of the bowel for the matter. Use of baskets or retrieval nets allows endoscopic removal of such impacted batteries. These batteries usually pass on along the GIT if beyond the oesophagus and only those remaining in the stomach longer than 48 hours, as seen in repeat radiographs, should be removed [13]. Once past the duodenum, 85% pass out of the body within 72 hours [14]. A radiograph every 3 to 4 days is adequate to assess the progress through the GI tract. Emetics are not beneficial in the management of disk battery ingestions and their use may lead to retrograde migration of batteries from the stomach into the oesophagus [13].
Most of the published series demonstrated ingestion of smaller objects. Large object like the wrist watch have not been reported and even with the increasing amount of evidence for the use of endoscopic extraction of these foreign bodies, a surgical approach is often needed. The timing of such intervention is most important and decision made for surgical exploration or endoscopic retrieval should be made considering the size, location and the duration of the foreign body impaction. Prevention is still better than cure and it is advisable to teach parents about the possibility of such occurrences as the child grows and develops and to dissuade such behaviour, so that any morbidity can be avoided.
Learning Points
-
Foreign body impaction though common often goes undiagnosed
-
High index of suspicion in cases of small children presenting with acute abdomenEndoscopy and retrieval devices facilitate easy extraction of impacted oesophageal objects
-
Surgical exploration should be done for sharp or long objects or those that remain in same position for more than 48hours.
Author contributions
SC Performed the literature review and prepared the draft report
DK: Helped with preparation of the draft report and collection of data and interpretation of results
MZH: Helped with preparation of the report and collection of data and literature.
SPS: Conceived and designed the study, edited the manuscript and approved the final manuscript for publication.
All authors have seen the final manuscript and approve it for publication.
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical consideration
Written informed consent was taken from the patient’s legal guardian, a copy of the consent is available with authors.
Funding
None declared
References
[1]. Bronstein AC, Spyker DA, Cantilena LR Jr, Green JL, Rumack BH, Heard SE. 2007 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 25th Annual Report. Clin Toxicol (Phila). 2008 Dec. 46(10):927-1057.
[Pubmed]
[2]. Abbas MI, Oliva-Hemker M, Choi J, Lustik M, Gilger MA, Noel RA, et al. Magnet ingestions in children presenting to US emergency departments, 2002-2011. J Pediatr Gastroenterol Nutr. 2013 Jul. 57(1):18-22.
[Pubmed]
[3]. Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 1995; 41:39-51.[Pubmed]
[4]. Cheng W, Tam PK. Foreign-body ingestion in children: experience with 1265 cases. J Pediatr Surg 1999; 34:1472-6.[Pubmed]
[5]. Hachimi-Idrissi S, Come L, Vandenpias Y. Management of ingested foreign bodies in childhood: our experience and review of the literature. Eur J Emerg Med 1998;5:319-23 [Pubmed]
[6]. Panieri E, Bass OH. The management of ingested foreign bodies in children—a review of 663 cases. Eur J Emerg Med 1995;2:83-7.
[Pubmed]
[7]. Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 1995;41:39-51.
[Pubmed]
[8]. Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc 1995;41:33-8. [Pubmed]
[9]. Smith MT, Wong RK. Foreign bodies. Gastrointest Endosc Clin N Am 2007;17:361-82. [Pubmed]
[10]. Rosch W, Classen M. Fiberendoscopic foreign body removal from the upper gastrointestinal tract. Endoscopy 1972; 4:193-7.
[Google
Scholar]
[11]. Nelson DB, Bosco JJ, Curtis W, et al. Endoscopic retrieval devices. Gastrointest Endosc 1999; 50:932-4 [Pubmed]
[12]. Vizcarrondo FJ, Brady PG, Nord HJ. Foreign bodies of the upper gastrointestinal tract. Gastrointest Endosc 1983; 29:208-10 [Pubmed]
[13]. Litovitz EL, Schmitz BF. Ingestions of cylindrical and button batteries: an analysis of 2382 cases. Pediatrics 1992; 89:747-57 [Pubmed]
[14]. Litovitz TL. Battery ingestions: product accessibility and clinical course. Pediatrics 1985; 75:469-76.[Pubmed]

