Case Report

post therapy lymphocytic thyroiditis in a case of primary thyroid tuberculosis
1Kiran Agarwal 1Mona Bargotya 1Geetika Sharma 2Nitin Sood
- 1Departments of Pathology and.
- 2Radiodiagnosis, Lady Hardinge Medical College, New Delhi, India
- Submitted Sunday, June 15, 2014
- Accepted:Tuesday, September 23, 2014
- Published Friday, October 10, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Lymphocytic thyroiditis following anti- tubercular therapy for thyroid tuberculosis is extremely uncommon. Primary tuberculosis of thyroid gland itself is a very rare clinical entity even in countries where tuberculosis is endemic. Thyroid tuberculosis can rarely be associated with features of hyperthyroidism or hypothyroidism. The aim of presenting this case report is to emphasize that this clinical entity should be kept in mind while treating thyroid diseases especially in a country where the prevalence of tuberculosis is high as well as to gain a better understanding of the clinical characteristics, diagnosis and treatment of this rare condition.
Key Words
Thyroid tuberculosis, Thyroiditis
Introduction
Once considered immune from tuberculosis, thyroid gland is very rarely affected by tuberculosis. Till today only few case reports and case series of thyroid tuberculosis are being documented in world literature. In 1862, Lebert demonstrated the involvement of the gland in a patient with disseminated tuberculosis [1 2 3]. The first case of tubercular involvement of thyroid gland without any evidence of miliary or pulmonary tuberculosis was first reported by Bruns in 1893 [1 2 3].
Tuberculosis of thyroid is very rare even in countries where the prevalence of tuberculosis is high [4]. Possible attributable factors for the relative immunity of the thyroid gland from tubercular infection are the intact thyroid capsule; rich vascular and lymphatic supply; high iodine content of the gland; bactericidal activity of colloid and thyroid hormones; enhanced phagocytic activity of gland macrophages as seen during hyperthyroidism; and possible antitubercular role of thyroid hormone[2 3 5]. On clinical examination, suspicion of the thyroid nodule or swelling as being tuberculous is very remote because of the rare presentation, until and unless it has destroyed much of the thyroid gland and formed an abscess [1]. Herein, we are presenting a case of primary thyroid tuberculosis in a 24 year old asymptomatic female presenting with diffuse neck swelling who subsequently developed lymphocytic thyroiditis with hypothyroidism following anti tubercular therapy (ATT).
Case Report
A 24 years old female presented with slow, progressively increasing, diffuse midline neck swelling since last one year. There was no history of fever, malaise, weight loss or any other generalized symptoms. It was not associated with difficulty in deglutition or change in voice. On examination, there was a large globular midline cervical swelling measuring about 6x5cms which was firm in consistency, diffuse, non-tender and moved with deglutition (Figure 1).

Figure 1: Large globular midline cervical swelling measuring 6x5 cms
Overlying skin was normal and surface was smooth. There was no associated
lymphadenopathy or dyshormonogenesis. Clinically a diagnosis of diffuse goiter
was made in a euthyroid patient. Investigations revealed a normal hemogram and
chest radiograph.T3,T4, thyroid stimulating hormone (TSH) and thyroid peroxidase
(TPO) levels were normal. Ultrasonography revealed enlarged lobes, right lobe
measuring 7.6x2.4x2.3cms, left lobe measuring 3.6x1.6x1.4 cms. The entire
thyroid gland appeared heterogeneous with multiple hypoechoic cystic areas and
internal septations, suggestive of thyroid abscess (Figure 2)

Figure 2: USG of thyroid showing herterogenous thyroid gland with multiple hypoechoic cystic areas and internal septations.
USG guided Fine needle aspiration cytology (FNAC) was done from the swelling
and it yielded frank pus even after multiple passes. Smears showed very
occasional epithelioid cell granulomas against a caseous necrotic background
however no thyroid follicular cells were seen. Ziehl-Neelsen staining was
positive for acid fast bacilli (AFB) (Figure 3)
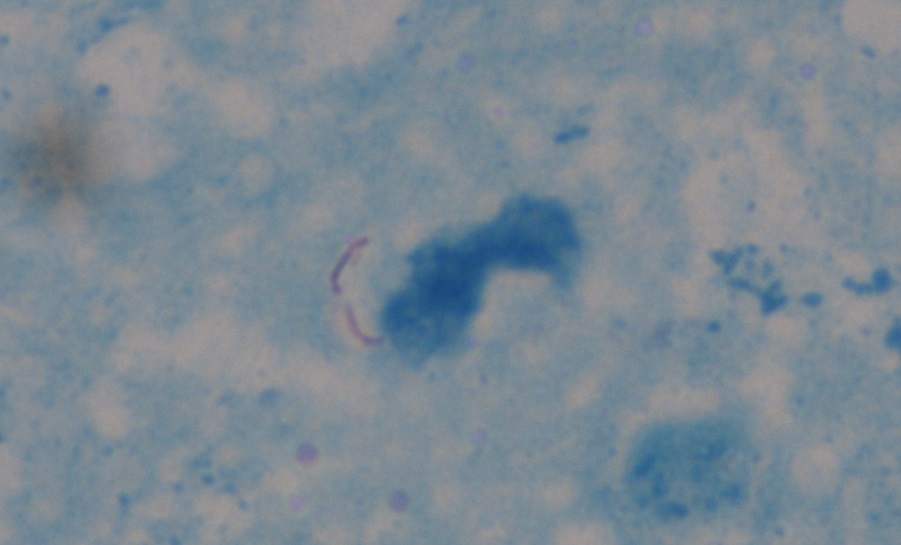
Figure 3: Ziehl- Neelsen stain showing acid fast bacilli in FNAC smear(x1000)
On this basis, a diagnosis of thyroid tuberculosis was made. However, the
patient had no past history or family history and history of contact. The
patient was started on anti-tuberculous therapy for 6 months. After completion
of the treatment the size of the swelling reduced but it never subsided
completely and slowly became tender. Hence, a repeat FNAC was performed. This
time, the cytological smears showed features of lymphocytic thyroiditis without
any evidence of tuberculosis (Figure 4). Following this thyroid function test was done which revealed a high TPO (>600 IU/mL, normal<34 IU/mL) and TSH (7.39, normal 0.34-5.6µ IU/ml) levels along with low T3(2.27, normal 2.5-3.9 pg/ml) and T4(0.56, normal 0.6-1.12 ng/dl) levels. ESR value was not raised throughout the clinical course.
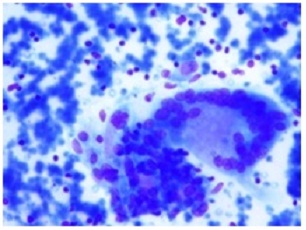
Figure 4: Post therapy FNAC smear showing presence of many lymphocytes along with a pseudogiant cell (Giemsax400)
Discussion
Tuberculosis of thyroid gland is an extremely rare disease with a frequency of 0.1%-0.4% [3 5 6] and primary form is still rarer. Despite a high incidence of tuberculosis in India, very few case reports are available. As per the literature tuberculosis of thyroid gland can be primary where no other organs are involved or secondary which occurs in association with tuberculous infection of other tissues or organs. Tuberculous infection spreads to the thyroid either by lymphogenous route, hematogenous route or by direct extension from adjacent organs [1 5]. Nevertheless, it is very difficult to differentiate primary form from secondary.
Clinically both primary and secondary type may present as: multiple minute lesions mimicking miliary involvement; glandular enlargement due to caseating granulaomas; cold abscess and sinus formation; chronic fibrosing tuberculosis simulating De Quervein’s thyroiditis; or rapid enlargement due to acute abcess formation mimicking carcinoma [2 3] Symptoms of thyroid tuberculosis are very non specific and variable. The patients are usually euthyroid with normal thyroid function tests but cases of hypothyroidism and hyperthyroidism are described [4]. Four variants of tubercular thyroiditis have been documented microscopically:1) multiple minute tubercles of miliary disease 2) solitary or merging tubercles 3) foci of caseous necrosis or cold abscess 4) cicatrized tubercle foci [2 3] .
Because of its rare occurrence, thyroid tuberculosis is usually not investigated. Many diseases can cause granulomatous inflammation of thyroid like granulomatous thyroiditis, fungal infection, sarcoidosis, granulomatous vasculitis and foreign body reaction. However, caseous necrosis is a cytologic finding specific to tuberculosis [2]. Seed, in 1939 proposed three criteria for the diagnosis of thyroid tuberculosis: 1) Demonstration of acid fast bacilli within thyroid; 2)A necrotic or abscessed gland; 3) Demonstration of tuberculosis focus outside. The third criteria is not essential for confirmed diagnosis [1 2 3]. FNAC with direct staining for AFB and culture of aspirated material for mycobacterium tuberculosis represent the procedures of choice for making appropriate diagnosis [7]. Histopathological examination of the surgical specimen is considered only when FNAC is negative. Demonstration of AFB by Ziehl Neelsen staining confirms the diagnosis, but this stain is often negative in tissue sections [2]. Sometimes bacteriological examination is not always achievable and in such cases polymerase chain reaction can be a reliable method to prove the presence of Mycobacterium tuberculosis within the thyroid [3].
Earlier, the treatment of thyroid tuberculosis consisted of antituberculous drugs combined with surgical removal of the affected parts of the thyroid gland or surgical drainage. But now it has been recognized that complete resolution usually follows an appropriate antituberculous drug treatment only. However, in cases with large abscess, surgical drainage or resection followed by antituberculous treatment is considered to be sufficient and further surgery is rarely required [6 7].
Very few cases are reported in the literature with features of thyrotoxicosis or hypothyroidism associated with tubercular thyroiditis [8 9 10].Thyrotoxicosis due to tuberculous thyroiditis is reported as a clinical syndrome of hyperthyroidism, which occurs generally at the beginning of glandular involvement due to its destruction followed by hypothyroidism due to extensive glandular destruction caused by caseous necrosis [6]. To the best of our knowledge no case of post therapy lymphocytic thyroidits occurring in a case of primary thyroid tuberculosis has been reported in the literature so far.
Conclusion
To the best of our knowledge there has been no case reported with occurrence of lymphocytic thyroiditis following ATT. To conclude, this case is presented to emphasize the importance of post therapy follow-up in a patient of thyroid tuberculosis. Merely diagnosing and treating the disease is not sufficient for proper patient care. FNAC with direct staining for AFB and culture of aspirated material for mycobacterium tuberculosis currently represent the important diagnostic procedures.
Key Message
Even in patients without any prior history and symptoms of tuberculosis, thyroid tuberculosis though rare, should be kept in mind in the differential diagnosis of midline cervical masses as failure to recognize this rare entity due to misleading clinical features may lead to inappropriate treatment
Ethical Consideration
Written informed consent was obtained from the patient for publishing this case report.
Conflict of Interests
The authors declare that there are no conflict of interests.
Authors’ Contributions
KA: Final diagnosis and edited final manuscript.
MB: Literature search and drafting of manuscript.
GS: Literature search and helped in interpretation.
NS: Provided clinical details and edited final manuscript.
Funding
None
Acknowledgement
None
References
[1]. Balasarkar D, Joshi MA, Dhareswar J, Satoskar RR, Awsare N, Mahey R, Kumar V. Primary thyroid tuberculosis. Bombay Hospital Journal. 1999; 41(2). http://www.bhj.org.in/journal/special_issue_tb/SP_13.HTM [Last accessed October 4, 2014]
[2]. Kataria SP1, Tanwar P, Singh S, Kumar S. Primary tuberculosis of the thyroid gland: a case report. Asian Pac J Trop Biomed. 2012 Oct;2(10):839-40. doi: 10.1016/S2221-1691(12)60240-8 [Pubmed]
[3]. Sengupta S, Pal S, Phukan JP, Bose K, Jana S. Tuberculosis of thyroid gland: A case report with review of articles. Open Journal of Pathology.2013;3:117-118
[4]. Zivaljevic V, Paunovic I, Diklic A. Tuberculosis of thyroid gland: A case report. Acta Chir Belg.2007; 107:70-72.
[5]. Gupta V, Boombak E, Tanwar P, Yadav H, Sen R. Tuberculosis of thyroid gland presenting as abscess. J Cytol Histol. 2012; 3:154.
[6] Majid U, Islam N. Thyroid tuberculosis: A case series and a review of the literature. J Thyroid Res.2011; 2011:359864.[Pubmed]
[7]Safarpor F, Hedayati-Omami MH, Mohammadi F, Hoda S, Safarpor D. Thyroid tuberculosis. Iranian Red Crescent Medical Journal.2007; 9(3) : 161-163.
[8] Kapoor VK, Subramani K, Das SK, Mukhopadhyay AK, Chattopadhyay TK. Tuberculosis of the thyroid gland associated with thyrotoxicosis. Postgraduate Medical Journal. 1985;61:339-340.[Pubmed]
[9]. Da Silva BP, Amorim EG, Pavin EJ, Martins AS, De Maltos PS, Zantut-Wittmann DE. Primary thyroid tuberculosis: a rare etiology of hypothyroidism and anterior cervical mass mimicking carcinoma. Arquivos Brasileiros de Endocrinologica e Metabologia. 2009; 53(4): 475-478.
[10] Luiz HV, Pereira BD, Silva TN, Veloza A, Maltos C, Manita I,Cordeiro MC, Raimundo L, Portugal J. thyroid tuberculosis with abnormal thyroid function-case report and review of the literature.Endocr Pract. 2013; 19(2):44-49[Pubmed]

