Case Report

Primay Gastric Tuberculosis
1Ruhi Dixit, 3Vineeta Srivastava, 2Mohan Kumar, 2Mridula Shukla, 3Manoj Pandey
- 1Departments of Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India
- 2Departments of Pathology, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India
- 3Departments of Surgical Oncology, Institute of Medical Sciences, Banaras Hindu University, Varanasi 221005, India
- Submitted: September 17, 2012
- Accepted: October 15, 2012
- Published: October 19, 2012
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Primary isolated gastric tuberculosis in absence of pulmonary tuberculosis in immune competent host is rare.
Case Report
We present here a case of 25 year old male who presented with persistent vomiting and was diagnosed as having tuberculosis on endoscopic biopsy examination. The patient was successfully treated with four drug anti tubercular treatment without any surgical intervention.
Conclusion
High degree of suspicion is needed as the tuberculosis may mimic numerous other benign and malignant diseases.
Introduction
Tuberculosis though rare in developed world is still a common disease in developing and underdeveloped countries. The incidence is rising in developing countries among high risk population [1]. Gastric tuberculosis in immune competent host specially in absence of pulmonary tuberculosis is extremely rare [2]. Use of chemotherapy for malignant lesions and gastrectomy for benign lesions has been proposed as a risk factor for gastric tuberculosis [3]. A retrospective cohort of 2215 patients with gastric cancer was matched with that of Centre of Disease Control, Taiwan’s data on tuberculosis [3]. In patients with gastric cancer without a history of gastrectomy and without previous anti-TB treatment, the overall crude incidence of new-onset TB was 788 per 100,000 person-years. Compared with the general population, the overall age-sex standardized incidence (SI) of tuberculosis in patients with gastric cancer was 134.3 (SI ratio [SIR]: 2.11, p < 0.05), 18% (4/22) with previous history of anti tubercular treatment recurred after gastric cancer diagnosis. Gastrectomy was a significant risk factor [SI] 159 (95% confidence interval [CI], 80-237, SIR: 2.5, p < 0.05), while chemotherapy was not statistical significance (SIR: 12.5, p > 0.05) [3].
The presentation of these patients is varied. Patients may present with hematemesis or other features of gastrointestinal bleeding [4,5,6,7,8], non healing chronic ulcer [9,10,11,12], mimicking malignancy [13,14,15], gastric perforation [16,17,18], pyrexia of unknown origin [19], and gastric outlet obstruction [20,21,22,23,24,25,26,27]. Thus a high index of suspicion is important in clinching the diagnosis. We report a case of gastric tuberculosis presenting as gastric outlet obstruction in a 25 year old male patient.
Case report
A 25 year old male presented with complains of vomiting for past one month. Initially the frequency of vomiting was 1-2 per day and it used to occur after 6-8 hours after ingestion of meals, however for past one week the frequency had increased to 4-6 and it used to occur within an hour of taking meals. Patient was able to take small amount of liquids without vomiting it out. There were no other complaints like fever, pain, or feeling of fullness. The patient was a known tobacco chewer, and the past history and family history were not contributory. On examination, the patients was lean built, pallor was present and there was no icterus, cyanosis, clubbing, pedal edema or generalized lymphadenopathy. Abdominal examination failed to reveal any lump or organomegaly, on percussion the epigestic area was dull and on auscultation a suction splash could be demonstrated. A clinical diagnosis of gastric outlet obstruction was made.
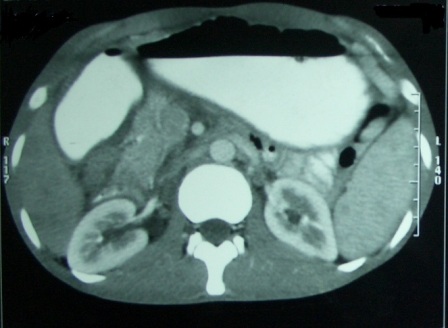
Figure 1: CT scan showing smooth distended stomach with partial outlet obstruction. No wall thickening or lesions are observed.
The hematological and biochemical investigations were normal, upper GI endoscopy revealed a distended stomach with residual food particles, no lesion could be identified. The pyloric region appeared to be hypertrophied and scope could not be negotiated in the duodenum. A punch biopsy was taken from the entro-pyloric part. Endoscopy was followed by computerized tomographic (CT) scan that revealed features suggestive of gastric outlet obstruction. No mass lesion within the gastric lumen or outside could be identified (Figure 1). The stomach was grossly dilated and passage of contrast was seen in small bowel suggesting a partial obstruction (Figure 2). The histopathological examination of the biopsy specimen revealed presence of epitheloid giant cells and granuloma with caseation (Figure 3), a diagnosis of primary gastric tuberculosis was made. Patient was started on four drug anti tubercular treatment with isoniazid, rifampin, pyrazinamide, and ethambutol. After two months of four drug treatment, pyrazinamide was stopped and patient was continued on three drug treatment for four months. Supportive treatment in form of anti emetics, and proton pump inhibitors were also started. Within two weeks of starting the treatment patient reported symptomatic improvement in vomiting and was able to take semi solid diet. The patient is currently disease free three years after treatment of primary gastric tuberculosis.

Figure 2: CT scan showing partial obstruction at the entropyloric region with distanded stomach and passage of contrast in small bowel.
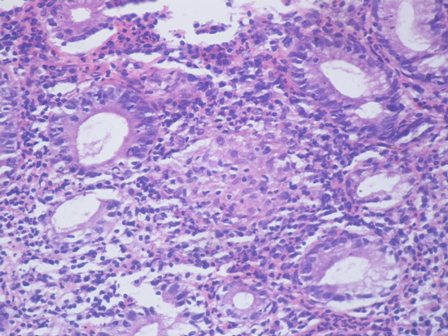
Figure 3: Photomicrograph showing granulomatous gastritis with epitheloid giant cells (H and E X400).
Discussion
Primary tuberculosis of the stomach is a rare disease characterized by hematemesis, non healing ulcer, and perforation with or without fever. Due to noncontributory clinical picture and imaging the diagnosis is usually difficult and depends on histological demonstration of epitheloid giant cell, granuloma and caseation [1]. When occurs its mostly in association with pulmonary tuberculosis or in immune-incompetent patients [28]. As mentioned earlier, the diagnosis is on histopathological examination of biopsy or resected specimen. On Ehrlich Ziehl-Neelsen staining, the presence of acid fast bacteria (AFB) can be demonstrated, the culture of the biopsy material can also yield AFB. However, in cases where the bacteria cannot be demonstrated and the classical tubercular granulomas are not present on histological examination, the diagnosis can still be made by using the polymerase chain reaction (PCR) [29]. In cases like ours where there are no superficial mucosal ulceration, or just thickening of mucosae is present Endoscopic ultrasound and guided FNAC, biopsy can help in obtaining the proper material and can aid in diagnosis [30]. A CT scan must be obtained as it aid to the diagnosis [31].
The treatment of primary gastric tuberculosis is same as that of pulmonary tuberculosis. However, certain situations may warrant a surgical intervention, e.g. obstruction or stenosis [20], bleeding [8,32,4] or perforation [16]. In some of these cases, the laparotomy may be required as an emergency procedure and the diagnosis of tuberculosis is made post hoc on examination of biopsy or resected specimen. These situations too warrant use of medical treatment of tuberculosis in the postoperative period with the same drugs and same schedule. If a surgical procedure is required, it usually depends on presentation and may require a partial or total gastrectomy with bypass [21] or bypass alone. What is the best drainage procedure in these cases is debatable; however, as in other cases a Roux-en-Y appears to be a better alternative over a loop procedure. There is concern over healing and fistula formation in these cases specially if the margins of resection contain active disease and hence some authors recommend minimum procedure if the diagnosis is achieved preoperatively [33].
Conclusions
The primary gastric tuberculosis is rare, it should be considered as a differential diagnosis in cases with features suggestive of chronic inflammation, stenosis or hyperplasia, obstruction or perforation, specially in areas that are endemic for tuberculosis. Tuberculosis can be a mimic of cancer and stromal tumors. It is also essential to differentiate it with other granulomatous lesions.
Authors’ contribution
RD: Prepared the draft manuscript.
VS: Literature search and preparation of manuscript.
MK: Contributed to the pathological part and wrote the manuscript.
MS: Editing of the manuscript for its scientific content.
MP: concept and design, and preparation of final manuscript.
Ethical considerations
Written informed consent was obtained from the patient for publication of this case report.
Conflict of Interest
The authors declare that there are no conflict of interests.
Founding
None
Reference
[1]. Giouleme O, Paschos P, Katsaros M, Papalexi F, Karabatsou S, Masmanidou M, Koliouskas D. Intestinal tuberculosis: a diagnostic challenge--case report and review of the literature. Eur J Gastroenterol Hepatol 2011; 23(11):1074-1077.[Pubmed]
[2]. Bandyopadhyay G, Lahiri S, Ghosh S. Gastric tuberculosis - a diagnostic dilemma. J Indian Med Assoc 2010; 108(12):875.[Pubmed]
[3]. Huang SF, Li CP, Feng JY, Chao Y, Su WJ. Increased risk of tuberculosis after gastrectomy and chemotherapy in gastric cancer: a 7-year cohort study. Gastric Cancer 2011; 14(3):257-265.[Pubmed]
[4]. Wig JD, Vaiphei K, Tashi M, Kochhar R. Isolated gastric tuberculosis presenting as massive hematemesis: report of a case. Surg Today 2000; 30(10):921-922.[Pubmed]
[5]. Sharma BC, Prasad H, Bhasin DK, Singh K. Gastroduodenal tuberculosis presenting with massive hematemesis in a pregnant woman. J Clin Gastroenterol 2000; 30(3):336.[Pubmed]
[6]. Rathnaraj S, Singh SK, Verghese M. Gastric tuberculosis presenting with hematemesis. Indian J Gastroenterol 1997; 16(3):110-111.[Pubmed]
[7]. Quantrill SJ, Archer GJ, Hale RJ. Gastric tuberculosis presenting with massive hematemesis in association with acute myeloid leukemia. Am J Gastroenterol 1996; 91(6):1259-1260.[Pubmed]
[8]. Goh SH, Ravintharan T, Sim CS, Chng HC. Gastric ulceration with acute bleeding from tuberculosis of the stomach--a case report. Ann Acad Med Singapore 1994; 23(6):903-906.[Pubmed]
[9]. Ishii N, Furukawa K, Itoh T, Fujita Y. Primary gastric tuberculosis presenting as non-healing ulcer and mimicking Crohn's disease. Intern Med 2011; 50(5):439-442.[Pubmed]
[10]. Cho YS, Kim JS, Kim HK, Ji JS, Kim BW, Chae HS, Han SW, Choi KY, Chung IS. A squamous metaplasia in a gastric ulcer scar of the antrum. World J Gastroenterol 2-28-2008; 14(8):1296-1298.[Pubmed]
[11]. Gubler Ch, Ehmann T, Meyenberger Ch. [Non-healing gastric ulcer]. Dtsch Med Wochenschr 7-25-2003; 128(30):1592-1594.[Pubmed]
[12]. Chetri K, Prasad KK, Jain M, Choudhuri G. Gastric tuberculosis presenting as non-healing ulcer: case report. Trop Gastroenterol 2000; 21(4):180-181.[Pubmed]
[13]. Kim SE, Shim KN, Yoon SJ, Jung SA, Kim TH, Yoo K, Moon H. A case of gastric tuberculosis mimicking advanced gastric cancer. Korean J Intern Med 2006; 21(1):62-67.[Pubmed]
[14]. Talukdar R, Khanna S, Saikia N, Vij JC. Gastric tuberculosis presenting as linitis plastica: a case report and review of the literature. Eur J Gastroenterol Hepatol 2006; 18(3):299-303.[Pubmed]
[15]. Okoro EO, Komolafe OF. Gastric tuberculosis: unusual presentations in two patients. Clin Radiol 1999; 54(4):257-259.[Pubmed]
[16]. Sharma D, Gupta A, Jain BK, Agrawal V, Dargan P, Upreti L, Arora V. Tuberculous gastric perforation: report of a case. Surg Today 2004; 34(6):537-541.[Pubmed]
[17]. Nagi B, Lal A, Kochhar R, Bhasin DK, Thapa BR, Singh K. Perforations and fistulae in gastrointestinal tuberculosis. Acta Radiol 2002; 43(5):501-506.[Pubmed]
[18]. Azzouz MM, Driss S, Kharrat J, Ayachi K, Ben Khelifa H. [Gastric tuberculosis apropos of a case discloed by a perforation]. Tunis Med 1990; 68(11):697-699.[Pubmed]
[19]. Salpeter SR, Shapiro RM, Gasman JD. Gastric tuberculosis presenting as fever of unknown origin. West J Med 1991; 155(4):412-413.[Pubmed]
[20]. Kshirsagar AY, Kanetkar SR, Langade YB, Potwar SS, Shekhar N. Duodenal stenosis secondary to tuberculosis. Int Surg 2008; 93(5):265-267.[Pubmed]
[21]. Manzelli A, Stolfi VM, Spina C, Rossi P, Federico F, Canale S, Gaspari AL. Surgical treatment of gastric outlet obstruction due to gastroduodenal tuberculosis. J Infect Chemother 2008; 14(5):371-373.[Pubmed]
[22]. Rehman A, Saeed A, Jamil K, Zaidi A, Azeem Q, Abdullah K, Rustam T, Qureshi N, Akram M. Hypertrophic pyloroduodenal tuberculosis. J Coll Physicians Surg Pak 2008; 18(8):509-511.[Pubmed]
[23]. Agrawal S, Shetty SV, Bakshi G. Primary hypertrophic tuberculosis of the pyloroduodenal area: report of 2 cases. J Postgrad Med 1999; 45(1):10-12.[Pubmed]
[24]. Woudstra M, van Tilburg AJ, Tjen JS. Two young Somalians with gastric outlet obstruction as a first manifestation of gastroduodenal tuberculosis. Eur J Gastroenterol Hepatol 1997; 9(4):393-395.[Pubmed]
[25]. Lath JR, Patel DK. Atypical case of tuberculosis of stomach presenting as gastric outlet obstruction. J Assoc Physicians India 1996; 44(4):286.[Pubmed]
[26]. Fernandez OU, Canizares LL. Tuberculous mesenteric lymphadenitis presenting as pyloric stenosis. Dig Dis Sci 1995; 40(9):1909-1912.[Pubmed]
[27]. Tromba JL, Inglese R, Rieders B, Todaro R. Primary gastric tuberculosis presenting as pyloric outlet obstruction. Am J Gastroenterol 1991; 86(12):1820-1822.[Pubmed]
[28]. Kalac N, Sahin S, Gozu A, Samurkasoglu B, Yilmaz Aydin L, Nazligul Y, Tezer A. [Very rare presentation of extrapulmonary tuberculosis: primary gastric tuberculosis]. Tuberk Toraks 2010; 58(3):293-296.[Pubmed]
[29]. Baylan O, Kilciler G, Albay A, Tuzun A, Kisa O, Dagalp K. Polymerase chain reaction based diagnosis of primary gastric tuberculosis in an 80-year-old woman: a case report and review of the literature. New Microbiol 2009; 32(2):217-221.[Pubmed]
[30]. Hussain T, Salamat A, Farooq MA, Hassan F, Hafeez M. Indications for endoscopic ultrasound and diagnosis on fine-needle aspiration and cytology. J Coll Physicians Surg Pak 2009; 19(4):223-227.[Pubmed]
[31]. Duan SY, Zhang DT, Lin QC, Wu YH. Clinical value of CT three-dimensional imaging in diagnosing gastrointestinal tract diseases. World J Gastroenterol 5-14-2006; 12(18):2945-2948.[Pubmed]
[32]. Weissman D, Gumaste VV, Dave PB, Keh W. Bleeding from a tuberculous gastric ulcer. Am J Gastroenterol 1990; 85(6):742-744.[Pubmed]
[33]. Padussis J, Loffredo B, McAneny D. Minimally invasive management of obstructive gastroduodenal tuberculosis. Am Surg 2005; 71(8):698-700.[Pubmed]

