Original Article

Epidemiology of Cervical Spine Lesions in the Multiply Injured Patient – Recent Data of the Traumaregister DGU®
1#Matthias Weuster, 1#Tim Klueter,
1Christina Hofgaertner, 1Peter Behrendt,
1Leif Menzdorf, 2Rolf Lefering, 1Stefanie Fitschen-Oestern, 1Andreas Seekamp, 1Sebastian Lippross, 3Trauma
Register DGU
- 1 Department of Trauma Surgery, University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany
- 2 Institute forResearch in Operative Medicine (IFOM), University Witten/Herdecke, Cologne, Germany
- 3 Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society (DGU).
- Submitted: Saturday, September 24, 2016
- Accepted: Thursday, November 3, 2016
- Published: Thursday, November 24, 2016
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
A cervical spine lesion (CSL) is common among polytrauma patients. Injuries may be life threatening. The clinical impact of CSL in multiple injured patients is the focus of this study.
Methods
A retrospective investigation on a total of 62,903 patients of the Trauma Register DGU® from 2009 and 2014 was performed. Preclinical and clinical data were analyzed.
Results
The cohort depicted the typical severity in polytrauma (mean age 51 ±21; mean ISS of 22 ± 12). 1,321 patients sustained a CSL with an AIS 4-6 including complete spinal cord syndrome. The number of male patients was more than twice as high as of female patients. Leading causes for CSL were car accidents, falls from <3m height and falls from >3m height. 12,023 patients were unconscious (GCS ≤8). The majority had a CSL of AIS <2. 406 unconscious patients suffered from a CSL with an AIS 4-6. Cardiopulmonary resuscitation (CPR) was performed in 2,000 patients in the preclinical setting and 1,003 patients received CPR in the resuscitation bay. Severe CSL (AIS 4-6) had a significantly lower blood pressure (102mmHg ± 46) and a significantly lower heart rate (74/min ± 34) than patients with less severe CSLs (AIS <2). Hospitalization was extended with the severity of CSL. Early mortality was high. More than half of the patients with CSLs (AIS 2-6) died within the first 24 hours. 404 patients were transferred to a rehabilitation facility.
Conclusion
Cervical spine lesions imply a peculiar element among polytrauma patients. Early mortality correlates with the severity of CSL. Rehabilitation facilities are mainly the end point.
Keywords
Cervical spine lesion, spinal cord injury, Glasgow Coma Scale, multiple trauma, TraumaRegister DGU® (TR-DGU)
Introduction
The cervical spine is first and foremost to be protected in the case of polytrauma. In rationale terms, a cervical spine lesion (CSL) has potentially life-threatening impact and may cause long-standing disabilities with poor neurological outcome [1, 2].
The mortality is reasonably high with around 17% due to spinal cord injury [2] after major trauma [3]. The annual incidence of SCI is around 29.5 persons per million worldwide [4]. Incidence rates of CSL dramatically increase in case of multiple injuries [5, 6]. In a large European cohort study the cervical spine was injured in almost 29% from a total of more than 33,000 patients with spinal injuries. Other studies unveil an annual incidence of spinal cord injuries (SCIs) of around 40 cases per million population in the United States [6, 7]. Therefore, numbers vary concerning incidence rates of SCI. Uttermost, the proper management of a CSL is essential as early diagnostics and adequate treatment are indicatory for the further clinical course. Thus, the pre-clinical application of cervical collars such as the “Stifneck” (Laerdal Medical GmbH, Puchheim, Germany) has been established in trauma guidelines [8- 10]. Though, cervical collars may be falsely applied and may harm pulmonary functions [8, 11, 12]. Still, the usage is reasonable. Neurological deficits and therefore spinal injuries need to be addressed in the course of initial treatment in the emergency department. Overlooking and miscalculation of cervical spine injuries determine poor clinical outcome [13, 14]. Thus, the correct understanding of a cervical spine lesion and its treatment are of essence within the management of multiple injuries. Anyhow, polytrauma treatment remains a multi-disciplinary approach [15].
Firstly, the intention of this study was to demonstrate the current epidemiology of CSL in polytrauma patients in the TraumaRegister DGU®. Secondly, we aimed to reveal the correlation of CSLs and the patients´ initial neurological status indicated by the Glasgow Coma Scale. Therefore, aspects of preclinical settings were considered and clinical course analysed.
Methods
The TraumaRegister DGU®
Trauma Society (Deutsche Gesellschaft für Unfallchirurgie, DGU) was founded in 1993. The aim of this multi-centre database is an pseudonymised and standardized documentation of severely injured patients. Data are collected prospectively in four consecutive time phases from the site of the accident until discharge from hospital: A) Pre-hospital phase, B) Emergency room and initial surgery, C) Intensive care unit and D) Discharge. The documentation includes detailed information on demographics, injury pattern, co morbidities, pre- and in-hospital management, course on intensive care unit, relevant laboratory findings including data on transfusion and outcome of each individual. The inclusion criterion is admission to hospital via emergency room with subsequent ICU/ICM care or reach the hospital with vital signs and die before admission to ICU. The infrastructure for documentation, data management, and data analysis is provided by AUC - Academy for Trauma Surgery (AUC - Akademie der Unfallchirurgie GmbH), a company affiliated to the German Trauma Society. The scientific leadership is provided by the Committee on Emergency Medicine, Intensive Care and Trauma Management (Sektion NIS) of the German Trauma Society. The participating hospitals submit their data pseudonymised into a central database via a web-based application. Scientific data analysis is approved according to a peer review procedure established by Sektion NIS. The participating hospitals are primarily located in Germany (90%), but a rising number of hospitals of other countries contribute data as well (at the moment from Austria, Belgium, China, Finland, Luxembourg, Slovenia, Switzerland, The Netherlands, and the United Arab Emirates). Currently, approx. 25,000 cases from more than 600 hospitals are entered into the database per year. Participation in TraumaRegister DGU® is voluntary. For hospitals associated with TraumaNetzwerk DGU® however, the entry of at least a basic data set is obligatory for reasons of quality assurance. All participating hospitals are described on the website of the TraumaRegister DGU® at www.traumaregister-dgu.de.
The present study is based on the evaluation of the standard documentation. It is in line with the publication guidelines of the TraumaRegister DGU® and registered as TR-DGU project ID 2014-028.
Data collection
The study was conducted over a five-year period from 2009 until 2014. We included all primarily admitted patients of the age ≥16yrs. Secondary transfers were not considered. The patients had an ISS ≥9 and (ICU/death). We included participating hospitals within Germany. The inclusion and exclusion criteria are displayed in (Figure 1) The severity was encoded as described by the Abbreviated Injury Scale (AIS). This score was established as an anatomical scoring system in 1969 and revised in 1990. Injuries are ranked on a scale of 1 to 6 from minor to unsurvivable lesions (AIS 9 = Died without further evaluation). Cervical spine lesions of an AIS ≥2 were considered. The description of AIS considering CSL is shown in (Table 1)..Inclusion- and exclusion criteria are shown in (Figure 1). Data were collected and classified by pre- and in-clinical phases. This retrospective analysis included trauma mechanisms, transporting devices, preclinical and clinical parameters. Preclinical treatment and clinical outcome were examined. The clinical course is focused on common terms and definitions of the TR-DGU: Glasgow Coma Scale (GCS 3-15), unconsciousness was defined as a GCS ≤8; shock was defined as a systolic blood pressure (RR sys) ≤90mmHg; multiple organ failure [16] is a failure of two or more organ systems; sepsis is defined by the ACCP/SCCM Consensus Conference Committee[17]. Mortality is a death caused by an incidence during the hospital stay. Outcome is defined by the patients´ discharge from hospital either home, rehabilitation or other hospitals.
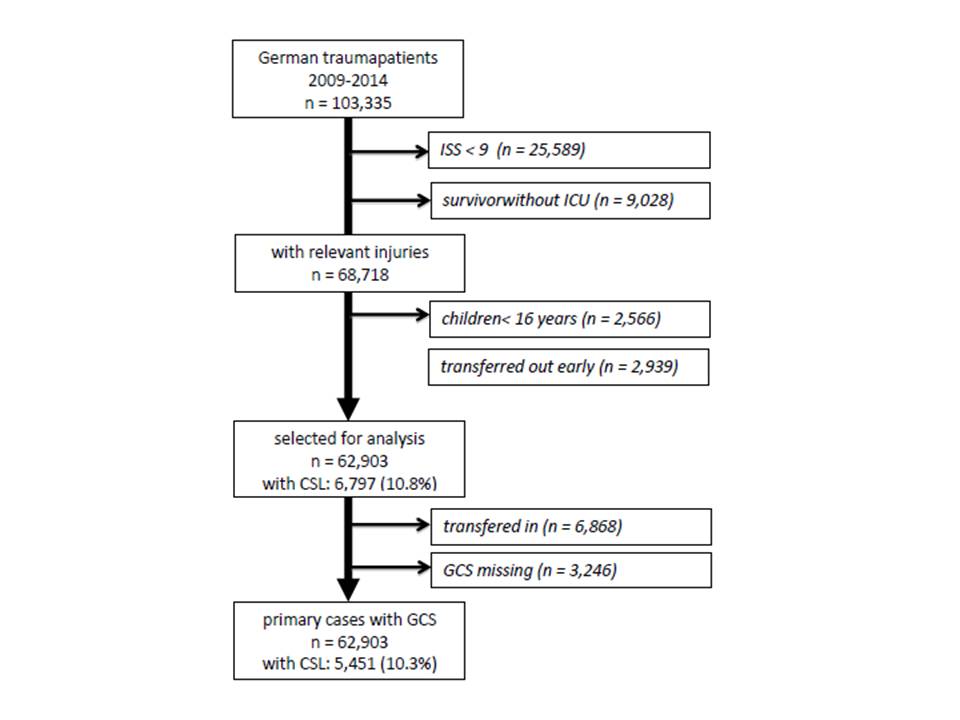
Figure 1: Consort diagram with inclusion and exclusion criteria.Data of TraumaRegister DGU®. Only German trauma centers were included.
Statistical analysis
We performed a descriptive analysis. Results are shown as mean with standard deviation. Statistical significance was defined as p<0.05.
Results
Epidemiology
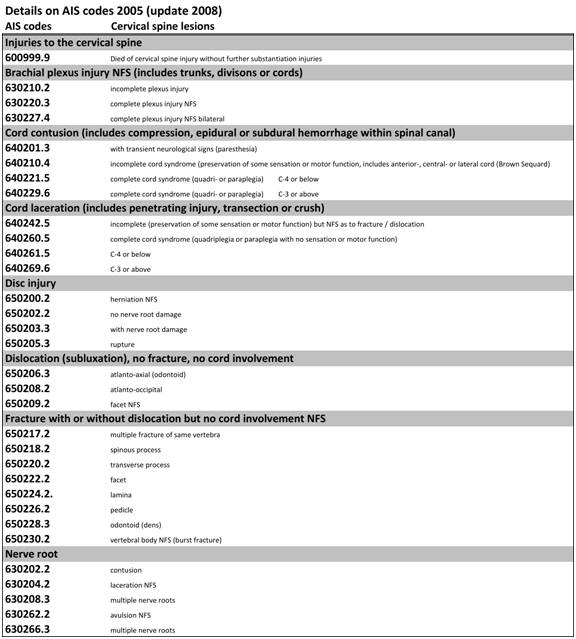
In a 5-year period from 2009 until 2014 one hundred and three thousand three hundred and thirty five(103,335) patients were documented in the TraumaRegister DGU®. 62,903 patients were included due to criteria (Figure 1). 6,797 (10.8%) patients had a documented cervical spine lesion (CSL) of AIS ≥2. Five thousand four hundred and seventy six (8.7%) patients had an AIS 2-3, which involved cord contusion with transient neurological signs. One thousand and three hundred and twenty one (2%) patients sustained a CSL of AIS 4-6, which included complete plexus injuries or a complete cord syndrome (Figure 2). In the collective of AIS 2-6, the mean age was 51 ±21 with a mean ISS of 22 ± 12. Considering all types of CSLs including AIS ≤2, the number of male patients was more than twice as high as the rate of female patients (44,728 vs. 17,803 patients).
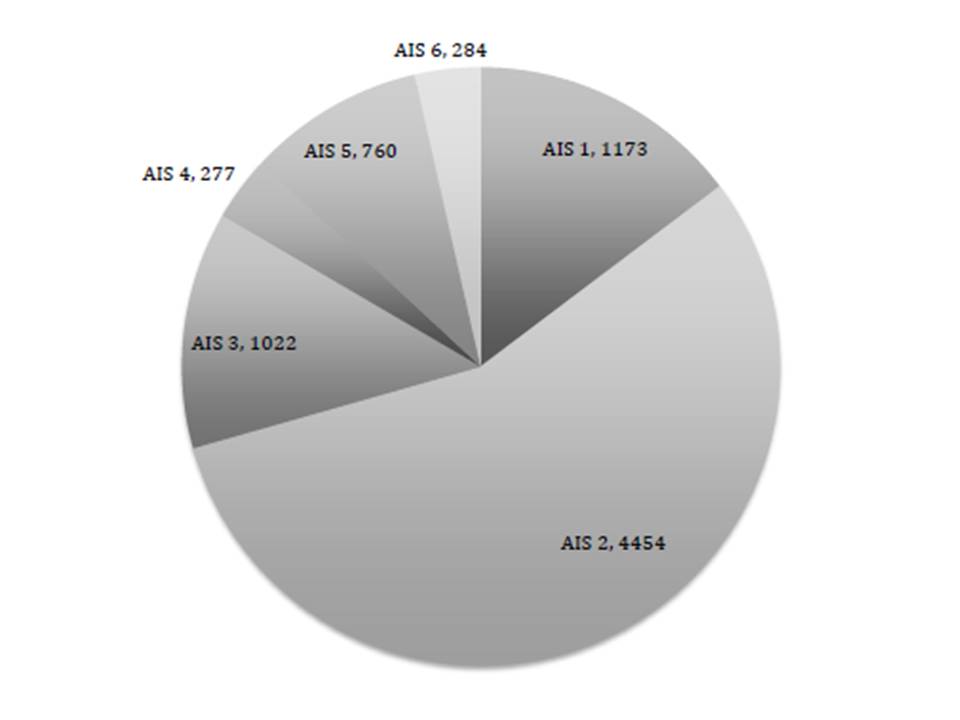
Figure 2:Frequency of cervical spine lesion (CSL) sorted by the Abbreviated Injury Scale (AIS 1-6). The rate is shown in absolute frequency. Data of TraumaRegister DGU®.
Preclinical settings and trauma mechanisms
mechanismsBlunt trauma prevailed penetrating trauma mechanisms (56,749 vs. 2,641 patients). In general, the leading three causes for CSL were car accidents (14,447 patients), falls from <3m height and falls from>3m height in the range of AIS 1-6. Serious injuries (AIS 4-6) were induced in descending order by falls <3m height, car accidents and falls >3m height. The majority of patients were transported by ground transporting systems. The Glasgow Coma Scale was documented in fifty two thousand seven hundred and eighty nine (52,789) patients. The GCS was>8 in 40,766 (77.2%) patients. Among this cohort; 36,954 patients had a CSL of AIS <2. 3,236 patients had a CSL of AIS 2-3 and 576 patients had a CSL of AIS 4-6. A total of twelve thousand and twenty three (12,023) (22,8%) patients were unconscious (GCS ≤8). 10,384 patients of those had a CSL of AIS <2. 1,233 patients had a CSL of AIS 2-3. 406 patients suffered from a CSL of AIS 4-6. The detailed spectrum of GCS and CSL is shown in Figure 3 Intubation was recorded in eighteen thousand four hundred and seventeen (18,417) patients. The majority had a CSL of AIS <2. 1,891 patients had an AIS 2-3 and 494 patients had an AIS 4-6. Cardiopulmonary resuscitation (CPR) was observed in two thousand (2,000) patients in the preclinical setting. 214 patients had an AIS 2-3 and 226 had an AIS 4-6. Monitoring the vital signs, severe CSLs (AIS 4-6) had a significantly lower blood pressure (102mmHg ± 46) and a significantly lower heart frequency (74/min ± 34)than patients with less severe CSL (AIS<). Preclinical volume management did not differ among the patients with CSLs (AIS <, AIS 2-3 and AIS 4-6).
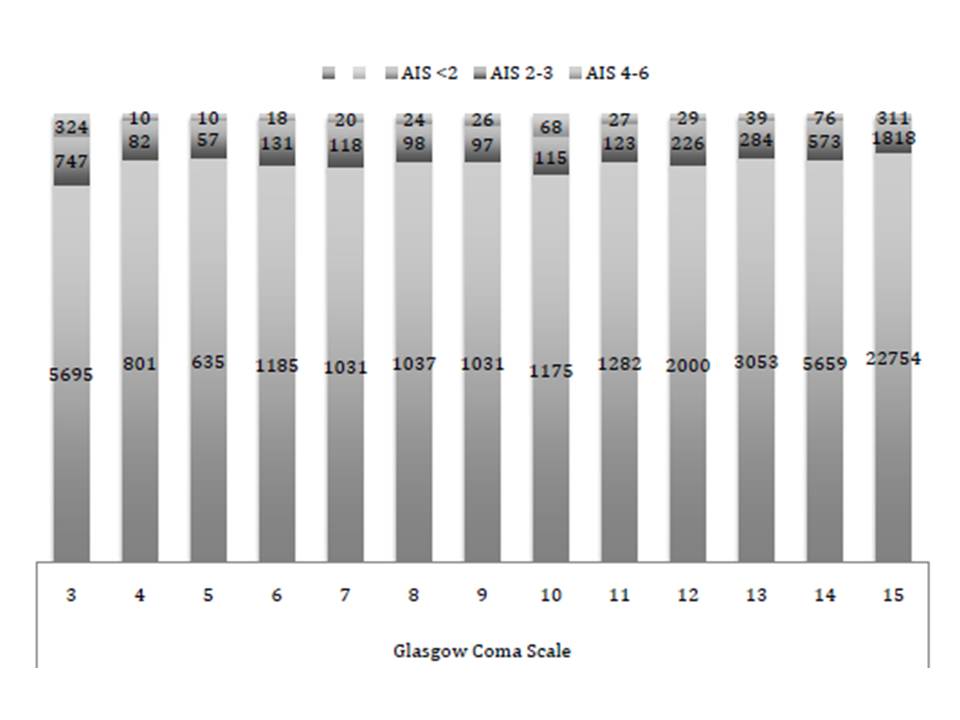
Figure 3: Distribution of Glasgow Coma Scale (GCS) considering the cervical spine lesion (CSL). CSLs are subdivided by AIS in three groups (AIS<2, 2-3, 4-6). X-axis: Scoring of GCS from 3-15; Y-axis: AIS in groups <2, 2-3, and 4-6. The numbers are displayed in absolute frequency. Data of TraumaRegister DGU®.
Injury characteristics
We screened the anatomic regions for the detailed array of injuries as given by the AIS. Head injuries were documented in 37,692 patients. In the occurrence of severe CSLs (AIS 4-6), five hundred and sixty five (565) patients had head injuries of an AIS 2-6. Eleven patients of those had head injuries of an AIS 6, such as open lesions and penetrating injuries (Figure 4). Spinal lesions (AIS 2) on thoracic and lumbar level were gathered. A thoracic spine lesion was present in 1,819 patients with a CSL of AIS 2-3 and 193 patients with a CSL of AIS 4-6. Concerning lumbar spine lesions, 912 patients had a CSL of an AIS 2-3 and 76 patients had a CSL of an AIS 4-6 (Figure. 5). Thoracic injuries (AIS ≥3) were found in more than twenty nine thousand patients with CSL (AIS <2-6). Most of whom (26,158) were little affected in CSL (AIS <2). 3,037 patients had an AIS of 2-3 and 420 had an AIS 4-6. Abdominal injuries (AIS ≥3) occurred in 664 patients with a CSL (AIS 2-6). Extremity lesions (AIS ≥3) coexisted in 18,885 patients who had a CSL with AIS <2-6 of whom the majority 17,300 suffered from AIS <2. 138 patients had an AIS 4-6.
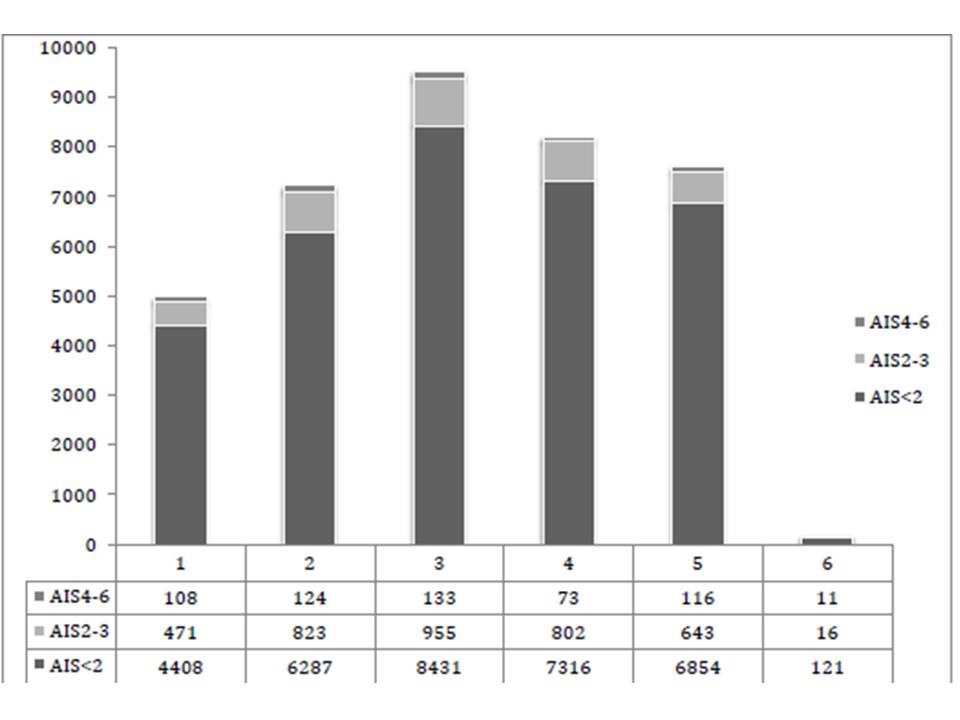
Figure 4: Frequency of head injuries in correlation to cervical spine lesions. X-axis: Head injuries in six columns AIS 1-6. Y-axis: The frequency of head injuries is displayed in three groups of cervical spine lesions (AIS<<2, 2-3, 4-6). Absolute frequency is displayed in the table below. Data of TraumaRegister DGU®.
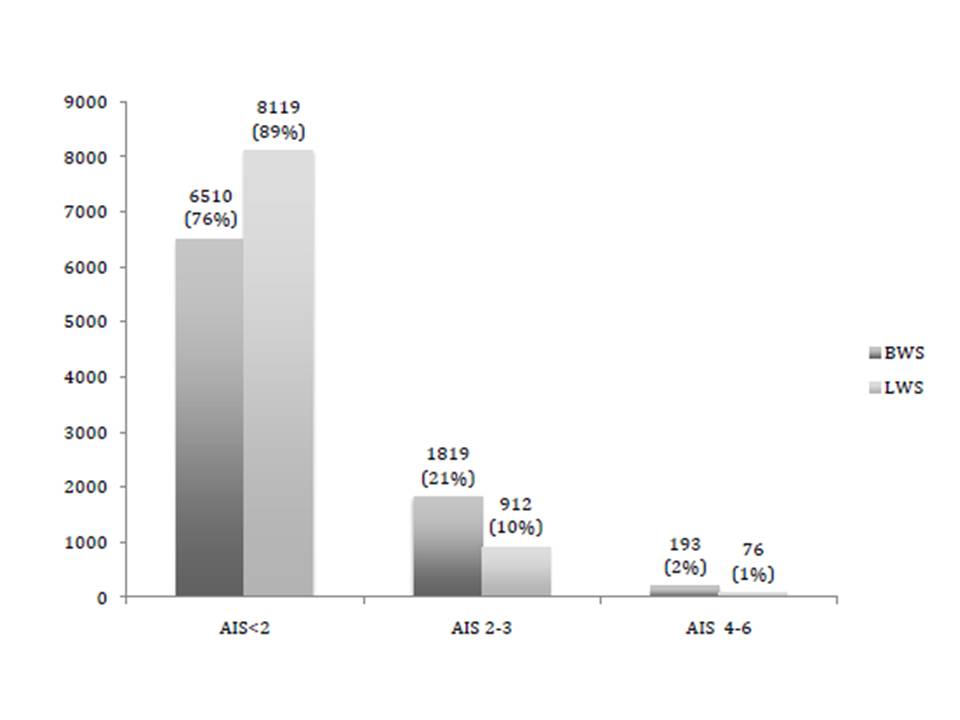
Figure 5: Frequency of thoracic and lumbar injuries in correlation to cervical spine lesions. X-axis: Thoracic and lumbar injuries in six columns AIS 2. Y-axis: The frequency and percentage of spinal injuries is displayed in three groups of cervical spine lesions (AIS<2, 2-3, 4-6). Data of TraumaRegister DGU®.
Clinical course and outcome
One thousand and three (1,003) patients received CPR in the shock room. Patients sustaining a CSL of an AIS 4-6 spent 69min ± 48 in the emergency room and received their first multi slice CT after around 20min. The majority of the patients (42,210) with CSLs (AIS <2-6) received a Multislice CT (MSCT)and 10,274 did not receive a MSCT. Hospitalization was extended with the severity of CSL. Patients with an AIS 4-6 stayed more than 26 days in hospital. Early mortality was rather high as more than half of the patients with CSLs (AIS <2-6) died within the first 24hours. In general, 7,670 patients died in the hospital whereas 45,118 patients could be discharged from the hospital. 90 patients (AIS 4-6) went home, whereas the majority (n=404) of severely injured patients went to rehabilitation facility
Discussion
Epidemiology
Roughly 18,000 patients are expected to be severely injured each year in Germany [18].This study illustrates the current epidemiology of cervical spine lesions in polytrauma taken from a large German cohort of 62,903 patients included over a five-year period. Considering the general data, our cohort was congruent in sex and age with other studies. The typical patient was male and young. 1,321 patients suffered from a severe cervical spine lesion of AIS 4-6. This grade of severity includes complete cord syndromes C-4 and below as well as C-3 and above with quadri- or paraplegia. Numbers on incidences of CSLs variegate in multiple injured patients due to the methods of study. This can be explained by regional and intercontinental differences on the one hand and by diverging inclusion criteria on the other hand [6, 19, 20]. A small number of 4% of all cervical spine lesions affect the traumatic atlanto-occipital and atlanto-axial dislocation [21]. Case reports are rare as such traumatic events are overlooked or end up lethally due to cardiorespiratory failure and spinal hematoma/rupture [22].. Large cohort studies on cervical spinal lesions i.e. spinal cord injuries result from worldwide trauma registers such as the Trauma Audit & Research Network from United Kingdom or the National Trauma Data Bank from the United States. Hasler et al. reported on 250,584 patients of whom 13% sustained spinal trauma, a rather large European study. 9.6% had spinal fractures/dislocations without neurological signs. Breaking down in subgroups the cervical spine was affected in 5,879 patients. They represent almost one-third in correlation to thoracic and lumbar spine fractures/dislocations. 1.8% suffered from spinal cord trauma among 250,584 patients and the CSL depicted the majority (n=2,039). Data were conducted over 11 years more than twofold in stretch of time in comparison to our study. But, patients included were less severe injured with median ISS 9 and a median GCS 15. Furthermore, the AIS had not been considered [3]. Almost 12% of our study group had a CSL. The general severity was heavier in these patients than in the previous mentioned study as measured by ISS. A very interesting study was published recently; around 6% had a cervical spine lesion in a prospective single-centre examination of more than 9,000 blunt trauma patients. The authors confirmed 5 predictors for cervical spine ligament injuries, such as 1) CT evidence of ligament injury; 2) Fracture pattern 'not' isolated transverse/spinous process; 3)Neurologic symptoms; 4) Midline tenderness and 5) GCS<5 [23]. Other studies clarified the rating of CSLs among multiple injured patients. Stephan et al. detected CSLs as the most frequent injuries amongst SCI. The severity of injury was described by the AIS as well as in our investigation. In declining order cervical spine lesions were distributed by AIS 5 followed by AIS 4, 6 and 3 [7]. The majority had a lesion of AIS 2 followed by AIS 3 and 5, baring lighter lesions in our study. These findings are affirmed by other examinations on SCIs [2]. Unfortunately, the TraumaRegister DGU® does not deliver detailed information on CSLs besides AIS. Still, clinical sequelae of CSLs are tremendous as injuries of the cervical spine are high in rates compared to the thoracic and lumbar spine. Thus, these facts still underline the need for a high quality management in trauma care. Trauma guidelines e.g. ATLS® have been successfully established [24, 25]. This system implements a quick assessment, which includes the obligatory application of a cervical collar. Cervical stabilizations are not quite uncritical as past studies showed. False handling and decrease in respiratory capacity were observed [8, 11].. Training skills are of essence and recommended [10].
Preclinical settings and Trauma mechanisms
Trauma victims have been mainly transported by ground than by air. Generally, transfer of patients from accident site to the next adequate trauma centre has been well organized in Trauma Networks, which has been established since years in Germany [26]. The trauma mechanisms were blunt despite a rising number of penetrating casualties in Northern Europe [27]. Falls from either <3m or >3m height as well as car accidents were the leading mechanisms [3 7]. It was not unexpected that car accidents imply a high relevance as shown by a study from the TraumaRegister DGU® [28]. In detail, precise mechanisms of CSLs have been examined by case reports and technical investigations e.g. in trampoline accidents in adults. Fractures and dislocations were described due to hyperflexions / -extensions of the cervical spine after landing [29]. Other studies showed the impact of a head velocity greater than 10ft/s (3m/s), which was enough to produce an injury to the lower spine between C5 and C7. This part is decisive as it forms the functional axis of rotation between the head and trunk. Tetraparesis or tetraplegia might follow in case of injury [30]. More typical CSLs are caused by diving accidents, which are provoked by flexion with or without axial compression [30]. Unfortunately, our database did not document these mechanisms of cervical trauma. We can only estimate the process of lesion in the cervical spine. Beyond, the type of lesion is decisive which was demonstrated in radiologic studies [1, 31]. MRI embodies the favourite tool [32]. Our study did not provide data on MRI. But, the majority of our cohort received CT respectively multi slice computer tomography (MSCT) by default. Indispensable, CT imaging has become a golden standard in acute trauma diagnostics and it is a fixed parameter within the TraumaRegister DGU® [33].
GCS, clinical parameters and outcome
patients is commonly captured by the Glasgow Coma Scale (GCS). This scale was established in Scotland in 1974 in order to verify patients´ consciousness [34]. Emergency care physicians apply this established parameter in trauma protocols worldwide. Most notably, the GCS (i.e. GCS ≤8) represents one criterion among four others defining the current term “polytrauma” in its revised version from 2014 [35]. In case of loss of consciousness a high alertness for spinal trauma is generally assumed. At least lumbar spine injuries can be excluded in patients with a GCS 15, with absence of pain or tenderness and without any influence of drugs/alcohol or preclinical sedative [36]. In particular, a cervical spine lesion might possibly correlate in its severity with the grade of consciousness. The anatomical location close to the respiratory centre and brainstem may be causative. Nevertheless, a one-to-one correlation is not completely feasible. Considering our data, we observed two peaks in the Glasgow Coma Scale (GCS 15 and 3) in the group of moderate to severe CSL (AIS 4-6). Sudden deaths were not listed, equivalent to an AIS 9 (=Died of cervical spine injury). One case report described one vertical atlanto-axial dislocation as a high cervical spine injury among 300 cervical CT scans. Two more patients died. The surgical treatment involved a fixation whereas traction was contraindicated [22]. Another study declared a high risk for cervical spine lesion in comatose patients (GCS 3-5) due to traumatic brain injury (TBI) [37]. Further studies elucidate the immense risk for cervical spine injuries as the typical patients´ characteristic include low GCS, frequently TBI and other severe injuries in polytrauma [23, 38]. Further on, the important vital signs (HF and Rays) were depressed as the severity of CSLs increased due to neurogenic shock. In our cohort heart frequency (HF) and systolic blood pressure (RRsys) were significantly lower in the CSLs of an AIS 4-6 than in AIS<2. Summers et al. analysed a complex hemodynamic flow after spinal cord injury. Lastly, they explained the neurogenic shock as a multifactorial process in case of trauma patients [39]. Volume management did not show significant differences among the AIS groups in CSLs in our study. Wood et al. justified pseudoephedrine as an effective adjunct in the medical treatment of a neurogenic shock [40]. Definitely, emergency care should be alert in recognising neurogenic shock and therefore adequate therapies should be initiated. Considering relevant injuries besides CSL, we observed quite a high number of coexisting head and thoracic injuries. These injuries are common in severely injured patients after polytrauma [41], and therefore these findings were not a surprise in our study. Moreover, length of hospital stay in patients with AIS 4-6 and the high rate of early mortality indicate the severity of injuries of such. This fact was underlined by the high rate of ISS (22 ± 12) in our cohort. Moreover, it implies high rates of sepsis, and multi-organ failure [42] as confirmed by our findings. Ultimately, the majority of severely injured patients in our study that were discharged went to rehabilitation facilities. But, we still do not know enough on recovery and on outcome of patients after rehab. As upper cervical spine lesions above C3 lead to restrictions in pulmonary functions and even death at scene [22, 43, 44], the lower cervical spine lesions rather cause restrictions concerning mobility in the upper extremities up to quadri- /paraplegia [31]. The recovery of these patients should be in the future focus.
Limitations
This study is a registry-based work, which involves incomplete and even missing data. Concerning the cervical spine, data is fragmentary on precise diagnosis. We could not differentiate on the exact level among CSLs. The Trauma Register DGU® only conducts the AIS. We could not specify the precise neurologic status in the emergency room. Moreover the exact neurologic recovery during hospital stay was not documented.
Conclusions
The cervical spine lesion is a profound injury after polytrauma. Preclinical settings indicate the severity. Strategies and accurate treatment are of essence. The impact of lesions is implied by depressed hemodynamic functions and even sudden death respectively early mortality. The coexisting injuries aggravate the patients´ clinical course. Furthermore, the hospital stay is complex and extended in such patients. Finally, quality of life and recovery after cervical spine lesions should be in focus.
Conflict of interest
The authors declare that there are no conflict of interest.
Authors´ Contribution
author and worked on this study. Christina Hofgaertner gathered data on polytrauma patients within our trauma center. Rolf Lefering provided the general data and analysis of the TraumaRegister DGU®. Leif Menzdorf, Stefanie Fitschen-Oestern and Peter Behrendt supported this study by gathering ideas, data and literature. Tim Klüter and Sebastian Lippross critically reviewed this work as supervisors and mentors. Andreas Seekamp is the head of department who made this work possible and supported our study at all times.
Ethical considerations
The study was approved by the Institute Ethics Committee.
Funding
None declared
References
[1] Martinez-Perez R, Paredes I, Cepeda S, Ramos A, Castano-Leon AM, Garcia-Fuentes C, Lobato RD, Gomez PA, Lagares A: Spinal cord injury after blunt cervical spine trauma: correlation of soft-tissue damage and extension of lesion. AJNR Am J Neuroradiol 2014, 35(5):1029-1034.
[Pubmed]
[Full text]
[2]. Scivoletto G, Farchi S, Laurenza L,
Tamburella F, Molinari M: Impact of multiple injuries on functional and
neurological outcomes of patients with spinal cord injury. Scand J Trauma Resusc
Emerg Med 2013, 21:42. [PubMed]
[Full
text]
[3]. Hasler RM, Exadaktylos AK, Bouamra O, Benneker LM, Clancy M, Sieber R, Zimmermann H, Lecky F: Epidemiology and predictors of spinal injury in adult major trauma patients: European cohort study. Eur Spine J 2011, 20(12):2174-2180.
[Pubmed] [Full
text]
[4]. Yue JK, Upadhyayula P, Chan AK, Winkler EA, Burke JF, Readdy WJ, Sharma S, Deng H, Dhall SS: A review and update on the current and emerging clinical trials for the acute management of cervical spine and spinal cord injuries - Part III.
J Neurosurg Sci. 2016 Dec;60(4):529-42. Epub 2015 Nov 24. [Pubmed]
[5]. Calancie B, Molano MR, Broton JG: Epidemiology and demography of acute spinal cord injury in a large urban setting. J Spinal Cord Med 2005, 28(2):92-96 [PubMed]
[6]. Lee BB, Cripps RA, Fitzharris M, Wing PC: The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord 2014, 52(2):110-116 [PubMed]
[7]. Stephan K, Huber S, Haberle S, Kanz KG, Buhren V, van Griensven M, Meyer B, Biberthaler P, Lefering R, Huber-Wagner S et al: Spinal cord injury--incidence, prognosis, and outcome: an analysis of the TraumaRegister DGU. Spine J 2015, 15(9):1994-2001 [PubMed]
[8]. Ala A, Shams-Vahdati S, Taghizadieh A, Miri SH, Kazemi N, Hodjati SR, Jalilzadeh-Binazar M: Cervical collar effect on pulmonary volumes in patients with trauma. Eur J Trauma Emerg Surg 2015.[PubMed]
[9]. Harris MB, Kronlage SC, Carboni PA, Robert KQ, Menmuir B, Ricciardi JE, Chutkan NB: Evaluation of the cervical spine in the polytrauma patient. Spine (Phila Pa 1976) 2000, 25(22):2884-2891; discussion 2892 [PubMed]
[10]. Pfeifer R, Pape HC: [Diagnostics and treatment strategies for multiple trauma patients]. Chirurg 2016, 87(2):165-175.[[PubMed]
[11] Kreinest M, Goller S, Rauch G, Frank C, Gliwitzky B, Wolfl CG, Matschke S, Munzberg M: Application of Cervical Collars - An Analysis of Practical Skills of Professional Emergency Medical Care Providers. PLoS One 2015, 10(11):e0143409 [PubMed]
[12]. Schikora N, Eysel-Gosepath K, Klunter H, Delank S, Guntinas-Lichius O: Influence of cervical spine stabilization via Stiff Neck on the postural system in healthy patients: compensation or decompensation of the postural system? Eur Arch Otorhinolaryngol 2010, 267(10):1623-1628.
[Pubmed]
[13]. Brown RL, Brunn MA, Garcia VF: Cervical spine injuries in children: a review of 103 patients treated consecutively at a level 1 pediatric trauma center. J Pediatr Surg 2001, 36(8):1107-1114.
[Pubmed]
[14]. Putz C, Schuld C, Akbar M, Grieser T, Wiedenhofer B, Furstenberg CH, Gerner HJ, Rupp R: Neurological and functional recovery in multiple injured patients with paraplegia: outcome after 1 year. J Trauma 2011, 70(5):1078-1085. [PubMed]
[15]. Claydon JH, Robinson L, Aldridge SE:
Patients' perceptions of repair, rehabilitation and recovery after major
orthopaedic trauma: a qualitative study. Physiotherapy. 2015 Dec 7. pii:
S0031-9406(15)03857-2. doi: 10.1016/j.physio.2015.11.002. [PubMed]
[16]. Moffatt SE: Hypothermia in trauma. Emerg Med J 2013, 30(12):989-996 [PubMed]
[17]. Tillotson SG. Introduction: Sepsis. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ, Committee ASCC: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. 1992.
Chest. 2009;136(5_suppl):e28. doi:10.1378/chest.09-2267. [Scopus]
[Pubmed]
[18]. Debus F, Lefering R, Frink M, Kuhne CA, Mand C, Bucking B, Ruchholtz S: Numbers of Severely Injured Patients in Germany. Dtsch Arztebl Int 2015, 112(49):823-829 [PubMed]
[19]. Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, Schopflocher DP, Voaklander DC: The epidemiology of traumatic spinal cord injury in Alberta, Canada. Can J Neurol Sci 2003, 30(2):113-121.[PubMed]
[20]. Lenehan B, Boran S, Street J, Higgins T, McCormack D, Poynton AR: Demographics of acute admissions to a National Spinal Injuries Unit. Eur Spine J 2009, 18(7):938-942 [PubMed]
[21]. Bohlman HH: Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am 1979, 61(8):1119-1142.[PubMed]
[22]. Pissonnier ML, Lazennec JY, Renoux J, Rousseau MA: Trauma of the upper cervical spine: focus on vertical atlantoaxial dislocation. Eur Spine J 2013, 22(10):2167-2175 [PubMed]
[23]. Duane TM, Young AJ, Vanguri P, Wolfe
LG, Katzen J, Han J, Mayglothling J, Whelan JF, Aboutanos MB, Ivatury RR et al:
Defining the cervical spine clearance algorithm: A single institution
prospective study of over 9000 patients. J Trauma Acute Care Surg. 2016
Sep;81(3):541-7. doi: 10.1097/TA.0000000000001151. [Pubmed]
[24]. Donaubauer B, Fakler J, Gries A, Kaisers UX, Josten C, Bernhard M: [Interdisciplinary management of trauma patients : Update 3 years after implementation of the S3 guidelines on treatment of patients with severe and multiple injuries].
Anaesthesist. 2014 Nov;63(11):852-64. doi: 10.1007/s00101-014-2375-y. [Pubmed].
[25]. Pape HC, Champion HR: Patient assessment in polytrauma: current trends rely on multiple parameters to improve the prediction of complications and mortality. Injury 2015, 46(10):1875-1877 [PubMed]
[26]. Ruchholtz S, Lefering R, Lewan U, Debus F, Mand C, Siebert H, Kuhne CA: Implementation of a nationwide trauma network for the care of severely injured patients. J Trauma Acute Care Surg 2014, 76(6):1456-1461 [PubMed]
[27] Stormann P, Gartner K, Wyen H, Lustenberger T, Marzi I, Wutzler S: Epidemiology and outcome of penetrating injuries in a Western European urban region. Eur J Trauma Emerg Surg 2016 [PubMed]
[28]. Lefering R, Paffrath T, Nienaber U: [The TraumaRegister DGU(R) as data source for monitoring severe injuries]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2014, 57(6):660-665.
[Pubmed]
[29]. Arora V, Kimmel LA, Yu K, Gabbe BJ, Liew SM, Kamali Moaveni A: Trampoline related injuries in adults. Injury 2016, 47(1):192-196.[PubMed]
[30]. Voland C, Vilarino R, Grabherr S, Lobrinus JA, Palmiere C: Fatal Cervical Spine Injury From Diving Accident. Am J Forensic Med Pathol 2015, 36(3):216-218.[PubMed]
[31]. Thorsen R, Binda L, Chiaramonte S, Dalla Costa D, Redaelli T, Occhi E, Beghi E, Ferrarin M: Correlation among lesion level, muscle strength and hand function in cervical spinal cord injury. Eur J Phys Rehabil Med 2014, 50(1):31-38.
[Pubmed]
[32]. Zohrabian VM, Parker L, Harrop JS,
Vaccaro AR, Marino RJ, Flanders AE: Can anatomic level of injury on MRI predict
neurological level in acute cervical spinal cord injury? Br J Neurosurg.
2016;30(2):204-10. doi: 10.3109/02688697.2015.1056089. Epub 2015 Jul 13. [Pubmed]
[33]. Huber-Wagner S, Lefering R, Qvick LM, Korner M, Kay MV, Pfeifer KJ, Reiser M, Mutschler W, Kanz KG, Working Group on Polytrauma of the German Trauma S: Effect of whole-body CT during trauma resuscitation on survival: a retrospective, multicentre study. Lancet 2009, 373(9673):1455-1461.
[Pubmed]
[34]. Teasdale G, Jennett B: Assessment of coma and impaired consciousness. A practical scale. Lancet 1974, 2(7872):81-84.[pPubMed]
[35]. Pape HC, Lefering R, Butcher N, Peitzman A, Leenen L, Marzi I, Lichte P, Josten C, Bouillon B, Schmucker U et al: The definition of polytrauma revisited: An international consensus process and proposal of the new 'Berlin definition'. J Trauma Acute Care Surg 2014, 77(5):780-786.
[Pubmed]
[36].Gill DS, Mitra B, Reeves F, Cameron PA, Fitzgerald M, Liew S, Varma D: Can initial clinical assessment exclude thoracolumbar vertebral injury? Emerg Med J 2013, 30(8):679-682.
[Pubmed]
[Full text]
[37].Tian HL, Guo Y, Hu J, Rong BY, Wang G, Gao WW, Chen SW, Chen H: Clinical characterization of comatose patients with cervical spine injury and traumatic brain injury. J Trauma 2009, 67(6):1305-1310.
[Pubmed]
[38]..Holly LT, Kelly DF, Counelis GJ, Blinman T, McArthur DL, Cryer HG: Cervical spine trauma associated with moderate and severe head injury: incidence, risk factors, and injury characteristics. J Neurosurg 2002, 96(3 Suppl):285-291.
[Pubmed]
[39]. Summers RL, Baker SD, Sterling SA, Porter JM, Jones AE: Characterization of the spectrum of hemodynamic profiles in trauma patients with acute neurogenic shock. J Crit Care 2013, 28(4):531 e531-535.[PubMed]
[40].Wood GC, Boucher AB, Johnson JL, Wisniewski JN, Magnotti LJ, Croce MA, Swanson JM, Boucher BA, Fabian TC: Effectiveness of pseudoephedrine as adjunctive therapy for neurogenic shock after acute spinal cord injury: a case series. Pharmacotherapy 2014, 34(1):89-93.
[Pubmed]
[41].Pfeifer R, Teuben M, Andruszkow H, Barkatali BM, Pape HC: Mortality Patterns in Patients with Multiple Trauma: A Systematic Review of Autopsy Studies. PLoS One 2016, 11(2):e0148844.[PubMed}
[42].Wafaisade A, Lefering R, Bouillon B, Sakka SG, Thamm OC, Paffrath T, Neugebauer E, Maegele M, Trauma Registry of the German Society for Trauma S: Epidemiology and risk factors of sepsis after multiple trauma: an analysis of 29,829 patients from the Trauma Registry of the German Society for Trauma Surgery. Crit Care Med 2011, 39(4):621-628.
[Pubmed]
[43].Garara B, Wood A, Marcus HJ, Tsang K, Wilson MH, Khan M: Intramuscular diaphragmatic stimulation for patients with traumatic high cervical injuries and ventilator dependent respiratory failure: A systematic review of safety and effectiveness. Injury 2016, 47(3):539-544.
[Pubmed]
[44]Zimmer MB, Nantwi K, Goshgarian HG: Effect of spinal cord injury on the respiratory system: basic research and current clinical treatment options. J Spinal Cord Med 2007, 30(4):319-330.
[Pubmed]
[Full text]

