Research

Severe Acute Injury Morbidity: A Study to Define Injury Near-Miss
1,2 Lateef O.A. Thanni, 3Sunday O. Sofola-Orukotan
- 11Department of Surgery, Olabisi Onabanjo University, Sagamu, Ogun State, Nigeria.
- 2Department of Orthopedics and Traumatology, Olabisi Onabanjo University Teaching Hospital, Sagamu, Ogun State, Nigeria
- 3Department of Orthopedics and Traumatology, Olabisi Onabanjo University Teaching Hospital, Sagamu, Ogun State, Nigeria
- Submitted: Friday, April 10, 2015
- Accepted: Thursday, April 16, 2015
- Published: Sunday, April 26, 2015
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Critical incident audit of trauma care is traditionally performed by mortality audits which is inadequate to describe morbidity associated with injuries. The injury severity scores available are used to predict death as an outcome of treatment but are also unable to predict morbidity as a tool to improve care and aid policy making. There is still a need for a clinical injury assessment tool that can assess morbidity (by introducing the concept of severe acute injury morbidity or near-miss injury morbidity) and quality of trauma care in relation to available facilities.
Aims and objectives
This study was intended to confirm the relevance of the concept of severe acute injury morbidity (SAIM), describe the characteristics of patients with SAIM and describe the epidemiology of their injuries. It is hypothesized that SAIM will outnumber injury mortality.
Methods
This is a prospective descriptive study of a cohort of injured patients who develop acute complications that threaten life without resulting in death. No patient intervention was involved. Eligible patients were injured patients who develop organ system failure or management failure. Patients that were brought in dead were excluded.
Results
There were 118 severely injured patients out of a total of 1885 injured, with a M:F ratio of 3.4:1 and mean age 37.5 years. The mean injury-arrival interval was 3.2 hours. Only 32 patients (27.1%) received preadmission care of which only one was on-board an ambulance. The etiology of injury were road traffic crash (RTC) 86.4% and firearm injury 5.9% while specific trauma diagnoses were traumatic brain injury (TBI) 35.6% and fractures 26.3%. The mean systolic blood pressure (SBP), diastolic blood pressure (DBP), respiratory rate (RR) and heart rate (HR) were similar for patients that died and those with SAIM. HR range however were unrecordable – 140 beats/min and 24 – 128 beats/min respectively. A total of 141 SAIM markers were identified in the 118 severely injured patients. Eighty-nine occurred in the SAIM cases while 52 occurred in those that died (Chi square = 0.72, p = 0.4). The SAIM initiating factors were hypovolaemia 52.5%, TBI 25.4% and sepsis 1.7%. The incidence of mortality and severe acute injury morbidity (near-miss injury) were 2.1% and 4.1% of all injured patients respectively while SAIM index was 339 per 1000 severely injured. The mortality indexes for near-miss initiating factors were 47% for TBI, 42.9% for respiratory distress, 30% for hypovolaemia and 12% for life saving surgery.
Conclusion
Severe acute injury morbidity occurs twice as often as trauma deaths. Trauma deaths may be associated with heart rate <25 or >128 beats per minute, injury-arrival interval greater than an hour and the presence of multiple near-miss injury markers. The most important near-miss injury initiating factors are TBI, respiratory distress and hypovolaemia. Cases of SAIM outnumbers trauma deaths by two to one
Key words
severe acute injury morbidity; near-miss injury morbidity; mortality index; trauma; injury; near-miss injury marker; quality of care; initiating factors
Introduction
Injury is the leading cause of death among people 5 to 44 years of age[1] and accounts for a significant proportion of all deaths. Trauma death range from 2% to 32% in prevalence [2, 3]. Trauma affects mainly, persons in the productive age group; hence the societal burden in terms of disability and premature death is enormous. Head injury (traumatic brain injury – TBI) and multiple injury are known to be the most important causes of trauma death [2, 3]. However, haemorrhage is a leading specific cause that is responsible for 30% to 40% of trauma related deaths despite improvements in trauma care [4, 5].
Advances in pre-hospital and in-hospital management of injured persons have no doubt reduced mortality from trauma in some countries. However, the number of injured persons, especially from road crashes is increasing globally particularly in rapidly motorizing countries. Disability and mortality from injuries are therefore increasing in many communities, making them contemporary subjects. Audit of trauma related death is the traditional method of assessment of the quality of trauma care. Different injury assessment tools exist, commonly to assess anatomic injury severity [6] (such as abbreviated injury score AIS, and injury severity score ISS, new injury severity score NISS and anatomic profile AP) while some include physiological injury assessment in addition to anatomic injury severity (such as TRISS). These scores generally are used to predict death as an outcome rather than describing morbidity, as a tool to improve care and aid policy making.
Due to current emphasis on quality of care, some hospitals have introduced quality indicators or audit filters. Quality indicators or audit filters constitute a mechanism for assessing and improving quality of care. These filters are clinical processes or outcomes of care which occurrence define or indicate unfavorable deviation from normal or standard (timeliness or appropriateness of care). There are few studies that can enable conclusions of the effectiveness of audit filters in improving quality of care of patients with major traumatic injuries [7]. A comprehensive systematic review by Stelfox
et al., [8] identified 1572 published quality indicators and was able to categorize them into 8 groups. Their review concluded that the evidence to support these indicators as a measure of quality of trauma care is not strong. More research is therefore required to fill knowledge gaps (in quality of trauma care) as well as identify and validate some indicators or filters to serve as globally acceptable measures of quality of trauma care. Traumatic injuries represent a heterogeneous collection of trauma conditions; hence the numerous indicators or filters that have been proposed to audit quality of trauma care. Further research is needed to define broadly applicable tools for describing morbidity and measuring quality of trauma care.An injury assessment tool that is easy to use in clinical practice, incorporating assessment of specific organ dysfunction as well as surgical intervention will greatly aid trauma audit especially when such tool also look at facility dysfunctions as measures of quality of trauma care.
Severe acute morbidity (SAM) or near miss morbidity is a concept that is established for assessing quality of obstetric care [9]. According to Mantel
et al., [10], cases of severe acute maternal morbidity outnumber maternal deaths by about five times, using a defined set of clinical criteria. Unlike audit of maternal deaths, audit of near miss maternal morbidity highlights the true burden of maternal morbidity. Audits of injury have shown that road crashes are the most prevalent cause while deaths results most often from head injury and multiple injury [2, 3, 11]. However, a lot of preventable deaths occur in the emergency room due to deficiencies in emergency treatment of injured persons. As many as 30% to 70% of trauma deaths may be preventable. Adapting the concept of near miss to assessing injured patients, the characteristics of severe acute injury morbidity (SAIM) and injury mortality can be described and the relationship between them defined
The aim of this study was to define the characteristics of severe acute injury morbidity (also described in this study as near-miss injury). It is possible that significant gaps exist in the management of the critically injured patients and such gaps, if they exist, may not be adequately described by traditional analysis of trauma related deaths.This study was intended to achieve the following specific objectives
a)confirm the relevance of the concept of severe acute injury morbidity
b)describe the characteristics of near-miss injured patients
c)describe the epidemiology of near-miss injuries
Patients and Methods
Setting and data collection
The study centre is a 420 bed teaching hospital facility, wholly government owned and funded. The Orthopaedic and Trauma service includes 30 adult and 6 paediatric definitive care beds. Acute trauma care setting is in the accident and emergency centre which has 5 resuscitation and 10 recovery beds. Although, almost all patients have no health insurance, acutely injured patients are admitted and treated fully for 24hrs, before relatives arrive. Dedicated doctors and nurses provide 24hrs coverage in this unit. Patients are admitted for definitive care or referred on request following resuscitation for major traumatic injuries.
This is a prospective descriptive study of a cohort of near-miss injured patients. Patients were recruited into the study from the accident and emergency unit and followed up through the trauma wards until discharge or death. All patients were seen in the accident and emergency unit and treatment was based on the discretion or judgement of the attending medical doctor and available facilities. Patients’ records were only reviewed for the purpose of this study as there were no study related interventions.
Every day, at least two study staff (a doctor and a nurse) reviewed the files and charts of all injured patients seen in the previous 24hrs, at a meeting with the Principal Investigator, to determine their eligibility for recruitment into the study. Eligibility for inclusion was determined by the clinical state of the injured patient or his / her need for specific treatment. These eligibility criteria or markers are categorized as organ system dysfunction and management based criteria. A data abstraction form (appendix) was used to record the personal details of patients, in addition to date and timing of injury events. Details of pre-hospital care, transportation to the study centre, surgical treatment, duration of emergency room stay and outcome of treatment were also documented. The specific outcome of care of interest include death or discharge from hospital. Patients that were dead on arrival were excluded from the study.
Definitions and criteria
A near-miss injury event is a sudden injury event that results in an acute complication that threatens the life of the injured individual but does not result in death due to luck or good quality trauma care. Therefore near-miss injury morbidity case is a patient who had a near-miss injury. Severe acute injury morbidity (SAIM) is synonymous with near-miss injury morbidity. To identify near-miss cases, we modified the “maternal near-miss” clinical criteria proposed by Mantel et al in 1998. We included emergency thoracotomy, emergency laparotomy and emergency amputation under management based eligibility criteria, (Table 1). The SAIM indicator or marker, therefore is the organ system dysfunction that complicates the injury event or management criteria (surgical intervention). The initiating factor is the complication that results in the series of events that threaten the patient’s life. All patients primarily identified by the near-miss indicators (and were therefore eligible for recruitment into the study) were defined as being severely injured. Of these, those who survive are the patients with severe acute injury morbidity. All patients that were dead on arrival were excluded.
|
Organ system dysfunction
|
Criteria
|
|
Cardiac
|
pulmonary edema, necessitating iv frusemide or intubation; cardiac
arrest
|
|
Circulatory
|
hypovolaemia requiring ≥ 5units whole blood or red cell transfusion;
systolic BP < 90mmHg for ≥ 60 mins
|
|
Immunologic
|
sepsis requiring ICU admission
|
|
Respiratory
|
intubation and ventilation for ≥ 60 mins; oxygen saturation < 90% for ≥
60 mins; intranasal oxygen administration for ≥ 60 mins
|
|
Renal
|
oliguria (400mls urine / 24hrs or less) that does not respond to iv
fluids or diuretics; serum urea ≥15 mmol/l; creatinine ≥ 400μmol/l
|
|
Hepatic
|
jaundice in the presence of hepatic injury
|
|
Metabolic
|
diabetic ketoacidosis; hypoglycaemic coma; thyroid crisis
|
|
Coagulation
|
acute thrombocytopaenia requiring platelet transfusion
|
|
Cerebral
|
coma lasting ≥ 12hrs; intracranial haemorrhage
|
|
Management-based criteria
|
|
|
Intensive care admission
|
for any reason
|
|
Emergency laparotomy
|
for blunt or penetrating abdominal injury
|
|
Emergency thoracotomy
|
for blunt or penetrating chest injury
|
|
Emergency amputation
|
for crush, mangled or gangrenous extremity
|
|
Anesthetic accidents
|
severe hypotension defined as systolic BP, 90 mmHg for ≥ 60 mins; high
spinal requiring intubation or failed intubation requiring anesthetic
reversal
|
Data analysis
Data were entered onto and analyzed using Epi Info version 3.5 (Centers for Disease Control and Prevention, USA). Descriptive statistics were performed using frequencies and averages. The incidence of SAIM and mortality were defined. The prevalence of SAIM (the ratio of SAIM to all injuries), prevalence of mortality (the ratio of deaths to all injuries) and injury – mortality index (the ratio of deaths to the sum of injuries and deaths) were defined. Severe acute injury mortality index was defined as a ratio of the total deaths to the sum of total deaths and total number of SAIM cases (as defined by Vandecruys
et al., [12]). Categorical variable were compared using Chi square and Fisher’s exact test as appropriate. The level of significance was set at a probability level of 5%.
Results
The study was conducted over an 18month period from November 2012 to April 2013, both months inclusive. During this period, 4820 patients were seen in the Accident and Emergency unit (A&E), of which 1885 were trauma patients. There were a total of 118 patients that were severely injured according to the study protocol and were recruited. Their mean age is 37.5 years (± 13.2) while the median and modal ages are 40 years and 36 years respectively .There was 91 (77.1%) males and 27 (22.9%) females with M: F ratio of 3.4:1. Forty of them eventually died and the remaining 78 patients were classified as severe acute injury morbidity (near-miss injury morbidity) patients, SAIM, (Table 2). A total of 141 near-miss markers were seen in the 118 severely injured patients. Eighty-nine occurred in the near-miss cases while 52 occurred in those that died, as shown in (Table 3).
|
|
SAIM (n = 78)
|
Died (n = 40)
|
p value
|
|
Age
|
|
|
|
|
Mean
|
36±13.4 years
|
40±12.5 years
|
|
|
Median
|
35 years
|
40 years
|
|
|
Mode
|
40 years
|
40 years
|
|
|
Range
|
1–70 years
|
15–83 years
|
|
|
Gender
|
|
|
|
|
Male
|
60 (76.9%)
|
31 (77.5%)
|
|
|
Female
|
18 (23.1%)
|
9 (22.5%)
|
0.87
|
|
M:F
|
3.3:1
|
3.4:1
|
|
|
Injury–arrival interval
|
|
|
|
|
Mean
|
3.3±6.5 hours
|
3±4.4 hours
|
|
|
Median
|
1 hour
|
1.5 hours
|
0.2
|
|
Mode
|
1 hour
|
1 hours
|
|
|
Range
|
0.3 hrs–48 hours
|
0.3 hrs–12 days *
|
|
|
Period of injury
|
|
|
|
|
Day
|
54 (69.2%)
|
34 (85%)
|
|
|
Night
|
14 (17.9%)
|
5 (12.5%)
|
|
|
Late night
|
10 (12.8%)
|
1 (2.5%)
|
0.1,df=2
|
|
*3 pts presented at
3,7,12 days respectively
|
|
Marker
|
SAIM
|
Died
|
p value
|
|
Organ dysfunction
|
|
|
|
|
Renal
|
0
|
0
|
|
|
Immunologic
|
0
|
1
|
|
|
Respiratory
|
3
|
7
|
|
|
Cerebral
|
18
|
13
|
|
|
Circulatory
|
42
|
20
|
|
|
|
63
|
41
|
|
|
Management criteria
|
|
|
|
|
ICU admission
|
1
|
1
|
|
|
Emergency amputation
|
4
|
3
|
|
|
Emergency laparotomy
|
10
|
1
|
|
|
Emergency thoracotomy
|
11
|
6
|
|
|
|
26
|
11
|
0.4
|
The average time of arrival in the A&E, after injury, was 3.2 hours (± 5.9). The median and modal injury-arrival intervals were one hour respectively. Three patients however presented 3 days, 7 days and 12 days respectively after injury. The injury event occurred during the daytime in 88 patients, at night in 19 and at late night periods in 11 patients.
Table 2 outlines the characteristics of the near-miss patients and those that died. The two groups were comparable in age, gender and period of injury. It is clinically important however, that the average time from injury to arrival is 1hour and 1.5 hours respectively, p = 0.2.
Preadmission care and transportation
Table 4 summarizes the characteristics of preadmission care received by the 118 patients. Eighty-six of them, representing 72.9%, did not receive any preadmission care. Of the remaining 32 patients that received preadmission care, only one received care on-board an ambulance while in transit to the hospital. Majority of this latter group of patients, 77.4% (n = 24) received initial care in a private clinic before referral to the study centre. Transportation to the hospital was in a car in 52 patients (44%), while a pick-up van was used in 47 (41%). An ambulance was used in 11 cases (9%) but none of them had advanced life support capability (ALS). The transportation was effected by the Federal Road Safety Corp (FRSC) team in 47 cases using mostly pick-up vans while relations were responsible in 42 instances using mostly cars
|
Preadmission care given
|
Frequency
|
|
Yes
|
32 (27.1%)
|
|
No
|
86 (72.9%)
|
|
Where preadmission care given
|
|
|
Traditional bonesetter
|
1 (3.2%)
|
|
General hospital
|
6 (19.4%)
|
|
Private hospital
|
24 (77.4%)
|
|
Type of preadmission care
|
|
|
Onboard ambulance
|
1
|
|
In-patient
|
31
|
|
Transportation to hospital
|
|
|
*APC
|
1 (0.8%)
|
|
Bus
|
7 (5.9%)
|
|
Ambulance
|
11 (9.3%)
|
|
Pickup van
|
47 (40.8%)
|
|
Car
|
52 (44.1%)
|
|
Transport to hospital
|
|
|
Friend
|
6 (5.1%)
|
|
Samaritan
|
7 (5.9%)
|
|
Police
|
11 (9.3%)
|
|
Relation
|
42 (35.6%)
|
|
FRSC
|
47 (39.8%)
|
|
Others
|
5 (4%)
|
|
*APC - Armored personnel carrier
|
Diagnosis and vital signs
The causes of injury or injury events are depicted in (Figure 1). Road traffic crash was the etiology in 102 patients (86.4%) followed by firearm injury in 7 (5.9%) patients. The trauma diagnoses, outlined in Table 5 shows that head injury or traumatic brain injury, 42 (35.6%) and fractures, 31 (26.3%) were the most frequent injuries associated with severe injury. Nine patients had injuries to the chest wall while 10 sustained abdominal injuries.
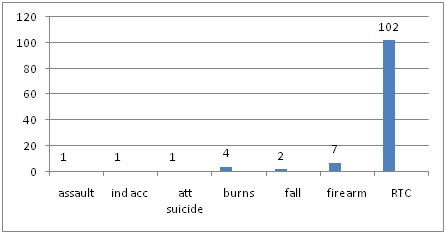
Figure 1. Aetiology of injury in 118 severely injured patients
att suicide – attempted suicide; indacc – industrial accident
|
Diagnosis
|
Frequency (%)
|
|
Traumatic brain injury
|
42 (35.6)
|
|
Fracture
|
31 (26.3)
|
|
Blunt chest injury
|
9 (7.6)
|
|
Burns
|
7 (5.9)
|
|
Blunt abdominal injury
|
6 (5.1)
|
|
Penetrating abdominal injury
|
4 (3.4)
|
|
Traumatic amputation
|
5 (4.2)
|
|
Spinal cord injury
|
4 (3.4)
|
|
Gunshot injury
|
4 (3.4)
|
|
Crush injury
|
2 (1.7)
|
|
Soft tissue injury
|
1 (0.8)
|
|
Others
|
3 (2.5)
|
|
Total
|
118
|
The mean systolic blood pressure (SBP) on admission was 101 (± 28) mmHg (range unrecordable to 180 mmHg). The mean diastolic blood pressure (DBP) was 63 (± 28) mmHg (range unrecordable to 140 mmHg), while the mean heart rate was 92 (± 21) beats / minute and mean respiratory rate 27 (± 6) cycles / minute.Table 6 shows that the near-miss injured patients and those that died had similar vital signs. Important differences exist however in the heart rate. A heart rate below 25 and above 128 per min appear detrimental to survival.
|
|
SAIM
|
Died
|
|
SBP mmHg
|
|
|
|
Mean
|
100.9 ± 30
|
101.3 ± 23.1
|
|
Mode
|
90
|
90
|
|
Range
|
unrec – 180
|
60 – 150
|
|
DBP mmHg
|
|
|
|
Mean
|
62.7 ± 20.6
|
63.7 ± 19.2
|
|
Mode
|
60
|
60
|
|
Range
|
unrec – 140
|
unrec – 90
|
|
RR cycles / min
|
|
|
|
Mean
|
26.8 ± 6.6
|
27.4 ± 5.8
|
|
Mode
|
24
|
24
|
|
Range
|
16 – 56
|
18 – 40
|
|
HR beats / min
|
|
|
|
Mean
|
91.2 ± 18.2
|
92.8 ± 25.9
|
|
Mode
|
100
|
88
|
|
Range
|
24 – 128
|
unrec - 140
|
Severe acute injury morbidity
Two groups of near-miss injury morbidity markers were employed in this study. Majority of patients, 97 (82.2%) had only one near-miss marker while 19 had 2 markers. The number of clinical diagnosis in the patients were one in 40 patients (33.9%), two in 52 patients (44.1%) and three in 26 (22%). Table 3 outlines the distribution of near-miss markers in those that died and the near-miss injured. Eighty nine markers (63%) were found in the near-miss cases and 52 in those who died (36%). The difference is statistically insignificant (Chi square = 0.72, p = 0.4). The ratio of organ system dysfunction to management criteria in the two groups of patients is 2.4:1 and 3.7:1 respectively. The prevalence of SAIM, defined as the ratio of SAIM (78) to the total number of injured patients (1885) is 4.1% or 41.3 per 1000 injured patients.
The factors initiating the severe injury (initiating factor), that is, the life threatening injury complications that results in organ or management dysfunction, are outlined in Table 7. The most frequent initiating factor was hypovolaemia, in 62 patients (52.5%) followed by TBI, in 30 patients (25.4%) while sepsis was the least common factor, seen in 2 patients (1.7%). This pattern of prevalence of initiating factors is present in the group of patients with SAIM and those who died. Only one patient had a co morbidity, a 70 year old male hypertensive who sustained TBI and fracture. The patient had one near-miss marker but died.
|
Factor
|
SAIM (%)
|
Died (%)
|
MI
|
p
|
|
|
Hypovolemia
|
43 (55.1)
|
19 (47.5)
|
30.6
|
0.6
|
|
|
Traumatic brain injury
|
16 (20.5)
|
14 (35)
|
|
46.7
|
0.1
|
|
Lifesaving surgery
|
15 (19.2)
|
2 (5)
|
11.8
|
0.07
|
|
|
Respiratory distress
|
4 (5.1)
|
3 (7.5)
|
42.9
|
0.7
|
|
|
Sepsis
|
0
|
2 (5)
|
100
|
0.1
|
|
|
|
78
|
40
|
|
|
|
Mortality
In all, 40 patients died. This represents 2.1% of all injured patients. The incidence of mortality and the number of near-miss criteria is as shown in Table 8. However, the percentage mortality shows incremental prevalence of mortality with increasing number of SAIM markers, almost double in the group with two compared to the group with one. Compared with the SAIM group of patients, there is no significant difference (p = 0.1). The age and gender characteristics of all patients and those that died are similar. SAIM mortality index is 33.9% or 339 per 1000 severely injured. The mortality index for the SAIM initiating factors, in table 7, indicates that TBI is more common cause of death (47%) compared to respiratory distress and hypovolaemia, 42.9% and 30% respectively. Mortality index for life saving surgery is 12%.
|
Severe acute injury morbidity (SAIM)
|
|
No of Criteria
|
Died (%)
|
Dama
|
Discharged
|
Admitted
|
Referred
|
Absconded
|
total
|
p
|
|
1
|
29(29.9)
|
9
|
19
|
5
|
34
|
1
|
97
|
|
|
2
|
10(52.6)
|
2
|
4
|
1
|
2
|
0
|
19
|
0.09
|
|
3
|
1(100)
|
0
|
0
|
0
|
0
|
0
|
1
|
|
|
4
|
0
|
0
|
1
|
0
|
0
|
0
|
1
|
0.1
|
|
Total
|
40
|
11
|
24
|
6
|
36
|
1
|
118
|
|
Discussion
There are several measures of quality of trauma care. Generally, these measures or instruments measure the degree or severity of anatomical injury or the body’s physiological response to injury. While they measure threat to life, the limitations to this approach to trauma care assessment are readily obvious. It is recognized that measures of threat to function and disability are equally or even more important to measure. The criteria for identifying severely or critically injured patients as in this study inherently accommodates for anatomical injury severity as well as physiological response to such injury by identifying organ system that malfunctions, possibly accommodating for comorbidity and age as confounders.
Injury is a contemporary issue worldwide. The attendant morbidity and mortality makes the subject relevant for continuing scientific inquiry. The nature and severity of injury however varies in different regions and communities, thus making objective study and comparison of patient groups difficult.
Prevalence of mortality is the usual scientific means of assessing outcome of care of injured patients and therefore quality of care. The shortcoming of the various scores for assessing the severity of injury lies in the difficulty of quantifying scientifically, the severity of injury. Even where this is taken care of, the quality of care also greatly vary in hospitals and surgical environments.
The present study evaluated a system of assessment of injury to patients taking into consideration 1)the severity of injury as a function of the physiological state of the body in response to injury and 2)the quality of care within the resources available in the care environment. This ultimately should make for ease of comparison of injury, survival outcome and quality of care all in one in different hospitals and surgical environments.
The patients with SAIM and dead patients in this study are comparable in terms of age, gender and time of day when accidental injury occurred. However, the average time to arrive in the emergency room is longer in those that died. This is suggestive of the need to improve transportation to appropriate hospitals within the golden period of one hour or start of adequate care or both. Although 11 patients were transported in an ambulance, only one received any care on-board. The government of the state introduced a few ALS ambulances close to the conclusion of this study to reinforce its emergency medical service (EMS). It is hoped that this might help with pre-hospital care of injured patients and transportation to the emergency room.
The most common organ system dysfunction in the study is circulatory system dysfunction. This is true for both SAIM and patients that died. This is followed by cerebral and respiratory systems dysfunction. This trend corresponds to the prevalence of initiating factors except that life saving surgery is the third most frequent initiating factor but the second most frequent dysfunction. Although respiratory dysfunction appear relatively unimportant as an organ system dysfunction and an initiating factor, it is the second most important cause of death, after TBI. This suggests the need for airway and oxygen therapy as the first priority for improvement, followed by blood transfusion therapy. Generally, the mortality indices are unduly high. However, the role of sepsis will become clear in a larger study.
This study identified injured patients who had threat to life (severe acute injury morbidity or near-miss injured) to be twice as many as those that died, 4.1% vs 2.1%. This highlights the bigger burden that injury morbidity truly is. Severe acute injury mortality index, 339 per 1000 (33.9%) severely injured, is very high and a better indicator, compared to mortality prevalence, of the challenge to healthcare givers and policy makers on the need to improve the various aspects of trauma care. Trauma death, as shown by our results appear to be associated with heart rate <25 or >128 beats per minute, injury arrival-arrival interval greater than an hour and the presence of multiple organ dysfunctions. The most important factors initiating complications that threaten life, TBI, respiratory distress and hypovolaemia suggests that the major challenges in clinical trauma care are oxygen therapy and airway management as well as blood transfusion and circulation maintenance.
Authors' contributions
LOAT: conception, design, data collection, analysis, manuscript writing, approval of final paper
SOS: data collection, review of manuscript, approval of final paper
Conflict of Interests
The authors declare that there are no conflicts of interests to declare.
Ethical Considerations
The Hospital Research and Ethics Committee (HREC) of the study centre approved the conduct of this research.
Acknowledgement
The authors gratefully acknowledge the contributions of the Musculoskeletal Diseases Research Group of OlabisiOnabanjo University Teaching Hospital. The contributions of all Medical Officers and Nursing Staff of the Accident and Emergency Unit of the hospital greatly aided the conduct of this study and are appreciated.
References
[1]Krug EG, Sharma GK, Lozano R: The global burden of injuries. Am J Public Health 2000, 90:523-526 [Pubmed]
[2]Thanni LO, Kehinde OA. Trauma at a Nigerian teaching hospital: pattern and documentation of presentation. African Health Sciences 2006; 6: 103-106 [Pubmed]
[3]Thanni LOA. Epidemiology of injuries in Nigeria—A systematic review of mortality and aetiology. Prehosp Disaster Med 2011; 26: 1-6 [Pubmed]
[4]. Spahn DR, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Gordini G, Stahel PF, Hunt BJ, Komadina R, Neugebauer E, Ozier Y, Riddez L, Schultz A, Vincent JL, Rossaint R; Task Force for Advanced Bleeding Care in Trauma.. Management of bleeding following major trauma: a European Guideline. Critical Care 2007, 11:R17 (doi:10.1186/cc5686) [Pubmed]
[5]. Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, Pons PT: Epidemiology of trauma deaths: a reassessment. JTrauma 1995, 38:185-193 [Pubmed]
[6] Beuran M, Negoi I, Păun S, Runcanu A, Gaspar B, Vartic M. Trauma scores: a review of the literature.Chirurgia (Bucur). 2012; 107:291-297 [Pubmed]
[7] Evans C, Howes D, Pickett W, Daqnone L. Audit filters for improving processes of care and clinical outcomes in trauma systems. Cochrane Database Syst Rev 2009; 4:CD007590 [Pubmed]
[8]. Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE. Quality indicators for evaluating trauma care: a scoping review.Arch Surg. 2010; 145:286-295 [Pubmed]
[9]Oladapo OT, Sule-Odu AO, Olatunji AO, Daniel OJ. Near-miss obstetric events and maternal deaths in Sagamu, Nigeria: a retrospective study. Reproductive Health 2005; 2:9 doi: 10.1186/1742-4755-2-9 [Pubmed]
[10]. Mantel GD, Buchmann E, Rees H, Pattinson RC. Severe acute maternal morbidity: a pilot study of a definition for near-miss. Br J ObstetGynaecol 1998; 105: 985-990 [Pubmed]
[11]. Aldawood AS, Alsultan M, Haddad S, Alqahtani SM, Tamim H, Arabi YM. Arabia. Ann 2012; 32:498-501 [Pubmed]
[12].Vandecruys H, Pattinson RC, Mcdonald AP, Mantel GD. Severe acute maternal morbidity and mortality in the Pretoria Academic Complex: changing patterns over 4 years. Eur J ObstetGynecolReprodBiol 2002; 102: 6 – 10 [Pubmed]

