Original Article

Rhabdomyosarcoma of Biliary Tract Misdiagnosed as Choledocal Cyst-Two Cases and Review of Literature
2 Sarita Chowdhary, 1 Dinesh Kumar, 1 Shiv Prasad Sharma
- 1Departments of Paediatric Surgery Institute of Medical Sciences, Banaras Hindu University, Varanasi, India
- 2General Surgery, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India
- Submitted: Monday, June 13, 2016
- Accepted: Friday, August 19, 2016
- Published: Friday, November 25, 2016
This is an Open Access article distributed under the terms of the Creative Commons Attribution License ((http://creativecommons.org/licenses/by/3.0)which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Rhabdomyosarcoma is a soft tissue malignant musculoskeletal tumour. It is a rare tumour in children but the most common cause of malignant obstructive jaundice in them. We present two cases of children who presented to us with obstructive jaundice and palpable liver. They were misdiagnosed as choledochal cyst on imaging studies; however, intraoperative and histopathological features confirmed the diagnosis of rhabdomyosarcoma. Mass excision and Roux en Y portoenterostomy was performed. Postoperatively, the patients were put on multimodal chemotherapy. This, being an uncommon entity, is being reported with a review of the available literature.
Keywords
Hepatic rhabdomyosarcoma, Choledochal cyst, Rhabdomyosarcoma in choledochal cyst, VAC
Introduction
Hepatic rhabdomyosarcoma (HRMS) is a rare lesion accounting for about 0.04% of all childhood cancers [1]. We report two cases of surgically managed HRMS that were preoperatively misdiagnosed as choledochal cyst. HRMS is considered the most common biliary tract tumour in children [2]. The median age of presentation is three years with a slight male preponderance. RMS of the biliary tract most commonly arises from the CBD [3].
Case Presentation
Case 1
A 4-year-old boy presented to the department of Paediatric Surgery of the University Hospital, Banaras Hindu University, with complaint of right upper abdominal pain, jaundice and passage of clay coloured stool. On examination, patient had icterus and palpable liver. Lab investigations showed raised bilirubin and raised Alkaline Phosphatase.
USG abdomen showed dilated CBD and intrahepatic biliary channels. CECT abdomen showed fusiform dilation of CBD (4.5 cm×2.3 cm). Intraoperatively, there was no evidence of choledocal cyst, and the lump appeared to be a biliary RMS. The tumor was carefully dissected from the portal vein and the hepatic artery. Excision of CBD with cholecystectomy with a roux en Y portoenterostomy was performed (Figure 1a,& b c). There was no evidence of metastasis or lymph node involvement. The HPE was suggestive of botryoid RMS. Post operatively; the patient was put on Vincristin, Adriamycin and Cyclophosphamide (VAC) chemotherapy. However after the first cycle, the patient did not come in follow up for one and half month. When patient returned he had evidence of jaundice. On USG, there was a mass at the porta, which appeared to be the recurrence. Considering this, the chemotherapy was changed to Ifosphamide and Etoposide, alternating with VAC. Following this chemotherapy jaundice was relieved and USG revealed decrease in the size of the mass at porta by 50 %. Patient is well even after three years. If the mass at porta will show evidence of increase, radiotherapy will be added to the treatment protocol.
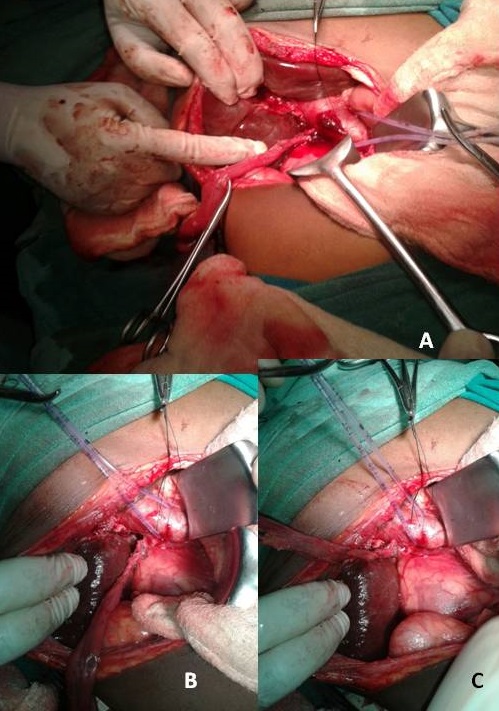
Figure 1: Intraoperative photograph showing the tumor (A); dissection from
portal vein (B), and Roux-en-Y anastomosis (C).
CASE 2
A 4-year old male presented with complaints of pruritus, epigastric pain , jaundice and passage of clay coloured stool. On physical examination, patient had jaundice and palpable liver. There was no ascites or palpable masses or splenomegaly. Laboratory studies showing raised bilirubin .USG abdomen showed a liver mass. CECT scan of the abdomen showed a non-calcified homogenously enhancing mass centered at the liver hilum. This mass had marked intrahepatic ductal dilatation and dilatation of the CBD. MRCP (Figure 2) showed fusiform dilation of entire common bile ducts s/o type 1 choledochal cyst.

Figure 2: MRCP showing fuciform dilation of entire common bile ducts
Patient was planned for surgery. Intraoperatively it was firm mass suggestive of rhabdomyosarcoma of biliary tract. Excision of the involved CBD, along with gallbladder was performed. The continuity was restored by a Roux en Y portoenterostomy. The histopathology was suggestive of botryoid RMS. Post operatively; the patient was put on Vincristin, Adriamycin and Cyclophosphamide (VAC) chemotherapy. Patient received three cycles of chemotherapy during which he was asymptomatic. After 3rd cycle he was lost to follow up.
Discussion
Tumours that arise from the biliary tree in early life are generally very rare [5]. HRMS represents about 0.5% of pediatric rhabdomyosarcoma and about 0.04% of all pediatric malignancy [6]. Since Wilks and Moxon reported the first case of HRMS in 1889, about 100 cases hae been reported till now [7, 8].
Common presentation of HRMS is jaundice associated with abdominal pain, vomiting and fever. This non-specific presentation makes differential diagnosis of HRMS difficult. Differential diagnoses include a long list with infectious hepatitis and choledochal cyst at the top. USG will demonstrate intrahepatic biliary ductal dilatation and an intraductal mass. Cystic areas may be seen in larger tumors and may represent areas of necrosis [7]. Because of this, it can have a radiologic appearance similar to choledochal cyst, especially if there is no local invasion. Imaging studies frequently misdiagnose it as choledochal cyst as noticed in our patient. However, it is suggested that for proper staging and planning of the management of the patient, both USG and CT scan may be needed [7]. There are certain reports where RMS was present within the choledochal cyst [9]. CT scan, by identifying the solid nature of the tumor, may help in differentiating it from choledochal cyst; however, it is not always possible, as seen in our patient. It can also help in staging the disease. On MRI T1-weighted images, RMS will present as a T1 hypointense and T2 hyperintense mass compared to the liver parenchyma.[10]. Post-contrast imaging is usually helpful since the presence of enhancement is a key feature that differentiates RMS from benign entities like sludge or debris. Intraoperative finding of soft white tissue bits also correlates well with the gross features described for RMS.
Immunohistochemical analysis is very useful in the diagnosis of embryonal RMS. More than 95 % of these tumours are positive for desmin [11]. In addition, nuclear staining with myogenin, a gene product that induces skeletal muscle differentiation, is useful in the diagnosis because of its specificity for RMS [11].
Differentiation between HRMS and choledochal cyst may be difficult even during pathological examination of the surgical specimen. Clinical and laboratory findings in both diseases are the same with no significant difference. Chemotherapy using Vincristine, dactinomycin, and cyclophosphamide can be used in case of extensive disease or R1 resection followed by second look surgery to evaluate resectability. Radiotherapy is indicated when chemotherapy fails or when there is postoperative residual tumour.
Various workers have advocated aggressive surgical intervention in a belief that reduction of tumour bulk affects the outcome [7]. However, there are reports indicating very good response either to chemo and radiotherapy, or delayed surgery after chemotherapy. Gross total excision is not always possible. Despite this, probably due the presence of favourable histology, the prognosis is relatively good [7].
The Intergroup Rhabdomyosarcoma Study Group (IRSG) has developed new protocols for children with sarcoma. For protocol purposes, patients are classified as low, intermediate or high risk [12] Staging of RMS is relatively complex [11] it includes assigning a local tumour group, staging and assigning a risk group. The estimated 5-year survival is 66%.
Conclusions
Radiologically RMS is often misdiagnosed as choledochal cyst. RMS should be considered in the differential diagnosis of choledochal cyst even if imaging is not suggestive for RMS. RMS need surgical excision and roux en y hepaticojejunostomy followed by chemotherapy. Redo surgery is indicated if residual disease remains which is followed by radiotherapy and chemotherapy as per need.
Ethical Consideration
Informed consent from the legal guardian of two cases had been taken. The copy of the consent is available with the authors.
Conflict of interest
No conflict of interest to declare.
Authors’ Contribution
DK: Conceived and designed the study, edited the manuscript.
SC: Performed the literature search and prepared the draft manuscript.
PS: Conceived and designed the study, edited manuscript for intellectual content and is the guarnteer of the manuscript.
References
[1].Chandra RS, Stocker JT. The liver, gallbladder, and biliary tract. In: Stocker JT, Dehner LP, editors. Pediatric pathology. Philadelphia: Lippincott; 1992
[2].Zampieri N, Camoglio F, Corroppolo M et-al. Botryoid rhabdomyosarcoma of the biliary tract in children: a unique case report. Eur J Cancer Care (Engl). 2006;15 (5): 463-6. Eur J Cancer Care (Engl) (full text) - doi:10.1111/j.1365-2354.2006.00683.x [Pubmed]
[3.Donnelly LF, Bisset GS, Frush DP. Diagnosis please. Case 2: Embryonal rhabdomyosarcoma of the biliary tree. Radiology. 1998;208 (3): 621-3 [Pubmed]
[4].McGahan JP, Goldberg BB. Diagnostic ultrasound. Informa Health Care. (2008) ISBN: 1420069780.
[5].Poggio PD, Buonocore M. Cystic tumors of the liver: a practical approach. World J Gastroenterol 2008;14(23):3616–20
[6.Davis GL, Kissane JM, Ishak KG. Embryonal rhabdomyosarcoma (sarcoma botryoides) of the biliary tree. Cancer 1969;24:333–42 [Pubmed]
[7].Sanz N, de Mingo L, Florez F, Rollan V. Rhabdomyosarcoma of the biliary tree. Pediatr Surg Int 1997; 12:200–1.
[8].Raney RB, Crist WM, Lawrence W, Lindberg RD. Rhabdomyosarcoma of the biliary tree in childhood. A report from the intergroup rhabdomyosarcoma study. Cancer 1985;56(3):575–81 [Pubmed]
[9].Patil KK, Omojola MF, Khurana P, Iyengar JK (1992) Embryonal rhabdomyosarcoma within a choledochal cyst. Can Assoc Radiol J 1992 Apr;43(2):145-8 [Pubmed]
[10].Chung EM, Lattin GE Jr, Cube R, et
al. From the archives of the AFIP: Pediatric liver masses: radiologic-pathologic
correlation. Part 2. Malignant tumors. Radiographics. 2011; 31: 483-507. [Pubmed]
[11].Morotti RA, Nicol KK, Parham DM et al (2006) an immunohistochemical algorithm to facilitate diagnosis and subtyping of rhabdomyosarcoma: the Children’s Oncology Group experience. Is J Surg Pathol 30:962–968?
[Pubmed]
[12].Ruymann FB, Raney RB Jr, Crist WM, Lawrence W Jr, Lindberg RD, Soule EH.Rhabdomyosarcoma of the biliary tree in childhood. A report from the Intergroup Rhabdomyosarcoma Study. Cancer 1985; 56: 575−581.[Pubmed]

