Case Report

Lymphoplasmacyte –rich Meningioma –A rare case report and review of literature
*Akriti Kashyap,*Tanushree Mukherjee, *Rahul Dev Chauhan
- *Department of Pathology, Command hospital Kolkata, India
- Submitted: Monday, September 4, 2017
- Accepted: Saturday, October 21, 2017
- Published: Monday, November 20, 2017
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Lymphoplasmacyte –rich meningioma is a very rare pathological entity which is included under WHO grade -1 meningiomas .These meningiomas are characterised by abundant lymphoplasmacytic infiltrate which overshadows the underlying the meningothelial component.
Case Presentation
:A 27 year old lady who presented with headache of 15 days duration and generalised tonic clonic seizures of one day duration. Her clinical, haematological and biochemical profile showed no abnormality. However MRI brain revealed a well –defined extra axial dura based mass in the right fronto-parietal convexity, possibly a meningioma. She was subsequently diagnosed as a case of lympho plasmacyte-rich meningioma,WHO grade -1 after histopathological examination.
Conclusions
Lymphoplasmacyte –rich meningiomas can have varied clinical manifestations and must be distinguished from other entities like idiopathic hypertrophic pachymeningitis and inflammatory pseudotumor which commonly affect the meninges and display a similar histopathological picture. Therefore correlation with MRI findings and further evaluation in the form of immunohistochemistry markers is required to reach a definitive diagnosis. However, neoplastic versus inflammatory nature of these meningiomas has to be ascertained and requires further research on the subject.
Key words
lymphoplasmacyte , meningioma , MRI, neoplasm, inflammatory
Introduction
Meningiomas are commonly encountered CNS neoplasms accounting for 30 % of all primary intracranial neoplasms [1] . According to WHO 2016 classification of tumors, three grades and 15 subtypes of meningiomas are recognized [2].
Lymphoplasmacyte rich meningioma, characterised by exuberant lymphoplasmacytic inflammatory cell infiltrate, is one of the rarest variants of meningioma [3]. This variant was first reported by Banerjee and Blackwood as a case of subfrontal tumor sharing features of meningioma and plasmacytoma in 1971 [4]. Lymphoplasmacytic meningiomas occur most commonly over cerebral convexities. Other sites include sphenoid ridges, olfactory grooves, parasellar regions, petrous ridges, tentorium and posterior fossa [3]. Here we report a case of a 24 year old lady who presented to Command Hospital ( Eastern Command ) with complaints of headache and generalised tonic –clonic seizures and after correlation with MRI and histopathology findings was subsequently diagnosed as a case of lymphoplasmacyte rich meningioma
Case Report
27 year old lady, wife of a serving soldier was admitted at Command Hospital Eastern Command ) Kolkata on 12 August 2016 with complaints of severe headache of 15 days duration and generalised tonic clonic seizures of one day duration. Her general condition was fair and vitals were stable. Clinical examination , particularly neurological examination revealed no significant abnormality. Her haematological profile was unremarkable. However, MRI brain showed a well defined extra axial dural based mass measuring 46.5x41x20 mm along the right fronto parietal convexity. The mass was seen causing inward buckling of grey –white matter interface with perilesional edema and sulcal effacement. No midline shift was seen. The lesion was isointense on T1W and heterogeneously hypointense on T2W and FLAIR sequences (Figure 1). Areas of blooming are seen within on GRE sequence. On post contast scan, intense homogenous enhancement of the mass along with “dural tail” was noted. Based on the MRI findings, a provisional diagnosis of meningioma was rendered and the patient was operated for the same.
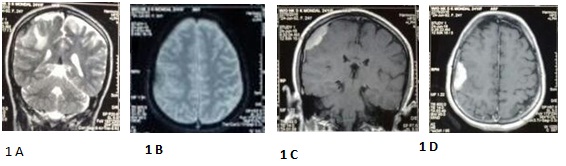
A well defined, extra-axial, oval shaped mass present at right fronto-parietal convexity. This mass is broad based at dura and measures about 38x20x34mm (APxTRxCC). Compared to the grey matter, this lesion is iso- to hypointense on T1W image (not provided here) and heterogeneously hypointense on T2W image (image 1a). On GRE (image 1b), this lesion shows blooming. The lesion is compressing the adjoining brain parenchyma and causing edema at adjoining white matter of fronto-parietal lobes (image1a). Post contrast (gadolinium), the lesion shows homogenous vivid enhancement (image 1c and 1 d). A characteristic dural tail is present at this lesion extending from its cranial and caudal aspects (image 1c). These features are typical of an intradural meningioma.
The specimen was subsequently sent for histopathological examination and consisted of multiple grey –white tissue bits ,aggregate amounting to 6 ml in volume. On microscopic examination, sections showed multiple bits of tissue displaying dense lymphoplasmacytic inflammatory infiltrate which was seen obscuring the underlying meningothelial cells that were focally seen to be arranged in whorls (Figure 2). There was no evidence of atypia or necrosis. Mitotic count was low (1-2/10 hpf). In view of the presence of brisk lymphoplasmacytic inflammation, a differential diagnosis of inflammatory pachymeningitis versus lymphoplasmacyte rich meningioma was considered. On immunohistochemistry, LCA was positive in lymphocytes while interspersed meningothelial cells showed positivity for EMA (Figure 3). Therefore, after correlating with MRI, histopathological and immunohistochemistry findings, a final diagnosis oflymphoplasmacyte –rich meningioma, WHO grade -1 was rendered.
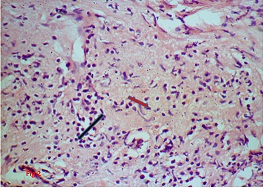
Figure 2: Photomicrograph showing dense lymphoplasmacytic inflammatory cell infiltrate (indicated by black arrow) obscuring the meningothelial component (indicated by red arrow)-H and E, 40x
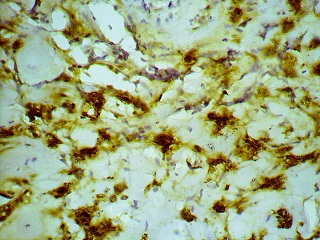
Figure 3: Photomicrograph displaying EMA positivity in interspersed meningothelial cells.(indicated by black arrow)
Discussion
Lymphoplasmacyte rich meningioma , a rare WHO grade -1 subtype, usually occurs in young and middle age patients without sex predominance. Lymphoplasmacyte rich meningioma can occur in a wide range of locations. While in our case lymphoplasmacytic meningioma was located in the right fronto –parietal convexity, Wang et al., [5] reported a case of cerebellar lymphoplasmacytic rich meningioma and Kanno H et al., [6] reported a case of lymphoplasmacytic meningioma in jugular foramen.(Table 1)
Authors
|
Sex/age
|
Site
|
Blood abnormalities
|
Perilesional edema
|
1)Gi
|
M/14
|
Left cerebellopontine angle
|
Hypergammaglobulinemia
|
-
|
2)Katayama
|
F/47
|
Left parietal lobe
|
absent
|
+++
|
3)Wang
|
F/70
|
Left cerebellar lobe
|
Hypergammaglobulinemia
And anaemia
|
absent
|
4)kanno
|
f/55
|
Right jugular foramen
|
absent
|
-
|
5)Present study
|
F/27
|
Right fronto parietal convexity
|
absent
|
++
|
Lymphoplasmacyte rich meningioma on MRI often shows evidence of peritumoral brain edema and dural tail signs which was also evident in the present case. Osawa et al., [7] reported that some histological variants, particularly the uncommon variants of WHO grade 1 meningiomas, including the lymphoplasmacyte rich meningiomas, are more often associated with edematous changes in the brain parenchyma than transitional, meningothelial and fibroblastic meningiomas which are the more common variants. Various theories have been proposed to explain the occurrence of brain edema in meningiomas. According to one theory proposed by Park et al., [8], Il-6 is an important mediator that leads to edematous transformation in the brain and was localized in the cytoplasm of tumor cells.
In a study by Hong da Zhu [9], out of the 62 cases of lymphoplasmacytic meningiomas reviewed by them, 13 cases (21 %) were associated with haematological abnormalities in the form of hyperglobulinemia and iron refractory anaemia. Gi et al., [10] reported a case of recurrent meningioma with hyperglobulinemia wherein the high serum immunoglobulins diminished after surgery and increased again after the tumour recurred. This led to the speculation that systemic hematological abnormalities and inflammatory cell infiltrate in meningioma are part of an unusual immunological response of the host individual [9].An important differential diagnosis is Idiopathic hypertrophic Pachymeningitis (IHP) which can pose a diagnostic challenge as it shows abundant lymphoplasmacytic inflammatory cell infiltrate and thickened dura admixed with islands of menigothelial cell, thereby mimicking a lymphoplasmacytic rich meningioma. It is pertinent to correlate with MRI findings in such cases as IHP usually shows diffuse plaque-like features while meningiomas present as a localized nodular thickening [9]
Other important differential diagnosis include intracranial Inflammatory pseudotumor (plasma cell granuloma) which most commonly presents as a meningeal mass and shows clinical and radiological similarities with Lymphoplasmacyte –rich meningioma. However, meningothelial component, highlighted by positive EMA and Vimentin markers, are absent in inflammatory pseudotumors [9] . In our case, interspersed islands of meningothelial cells showed positivity for EMA ((Figure 3).
Lymphoplasmacyte –rich meningioma is rare and usually associated with a favourable outcome. Surgical resection is the treatment of choice. However, whether this entity has an inflammatory origin or a neoplastic one is still uncertain and requires research on the subject.
Competing Interests
The authors declare that there are no competing interests.
Authors’ contribution
AK
:
carried out literature search and prepared draft manuscript.
TM:
conceived the study, participated in the design and edited the final manuscript.
RDC:
conceived the study, participated in the design and edited the final manuscript.
All authors have read the final manuscript and approved it for final submission.
Ethical Considerations
The written informed consent was taken from the patient and the copy of consent is available with the authors
Funding
None declared
References
[1]Claus EB, Bondy ML, Schildkraut JM, Wiemels JL, Wrensch M, Black PM.. Epidemiology of intracranial meningiomas. Neurosurgery 2005; 57: 1088-1095. PMID: 16331155 [PubMed]
[2]Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016 Jun; 131(6):803-20. doi: 10.1007/s00401-016-1545-1. Epub 2016 May 9. PMID: 27157931 [PubMed]
[3]Cambruzzi E, Thaís Amara da Costa de S; Silveira LC; Moreira C, dos Santos F. Lymphoplasmacyte-rich meningioma: a case report of a rare neoplasm. Jornal Brasileiro de Patologia e Medicina Laboratorial 2012; 48(3): 223-227. http://www.scielo.br/pdf/jbpml/v48n3/a12v48n3.pdf
[4]Banerjee AK, Blackwood W. A subfrontal tumour with the features of plasmocytoma and meningioma. Acta Neuropathol 1971; 18: 84-88. PMID: 5579381 [PubMed]
[5]Wang XM, Li FC, Lu MS, Hou QY, Zhang MY, Chen F. Lymphoplasmoacyte-rich meningioma: A report of two cases and review of literature. Central China Medical Journal. 2008;32:254–265.
[6]Kanno H, Nishihara H, Hara K, Ozaki Y, Itoh T, Kimura T, Tanino M, Tanaka S. A case of lymphoplasmacyte-rich meningioma of the jugular foramen. Brain Tumor Pathol. 2011 Oct; 28(4): 341-5. doi: 10.1007/s10014-011-0048-y. Epub 2011 Jul 2.
[PubMed]
[7]Osawa T, Tosaka M, Nagaishi M,
Yoshimoto Y. Factors affecting peritumoral brain edema in meningioma: special
histological subtypes with prominently extensive edema. J Neurooncol 2013; 111:
49-57. [PubMed]
[8]Park KJ, Kang SH, Chae YS, Yu MO, Cho
TH, Suh JK, Lee HK, Chung YG. Influence of interleukin-6 on the development of
peritumoral brain edema in meningiomas. J Neurosurg 2010; 112: 73-80. [PubMed]
[9]Zhu HD, Xie Q, Gong Y, Mao Y, Zhong P,
Hang FP, Chen H, Zheng MZ, Tang HL, Wang DJ, Chen XC, Zhou LF.
Lymphoplasmacyte-rich meningioma: our experience with 19 cases and a systematic
literature review. Int J Clin Exp Med. 2013 Aug 1;6(7):504-15. Print 2013. [PMC]
[10.].Gi H, Nagao S, Yoshizumi H,
Nishioka T, Uno J, Shingu T, Fujita Y. Meningioma with hypergammaglobulinemia.
Case report. J Neurosurg 1990; 73: 628-629. [PubMed]


