Case Report

Use of Natural Orifice for Specimen Extraction in Laparoscopic Solid Organ Surgery
Subhasis Misra, MD, MS, Brenten Popiel, BS, Digant Gupta, MD, MPH, Cathia Santos BA, Sybilann Williams, MD, Christopher Stephenson, DO
Cancer Treatment Centers of Americaâ, 2520 Elisha Ave., Zion, IL 60099, USA
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
One of the limitations of laparoscopic solid organ surgeries is making a relatively big incision for specimen extraction. This is often encountered with large tumors and in cases where morcellation of the specimen would distort the tissue architecture hindering pathological examination. This report highlights the use of a natural orifice for specimen extraction to avoid the above mentioned difficulty.
Case Report
A 34 year old female with Hodgkin’s Lymphoma underwent concomitant laparoscopic splenectomy for massive splenomegaly and laparoscopic assisted vaginal hysterectomy and bilateral salpingo-oophorectomy for menometrorrhagia. Given the significant size of the specimen, 17 x 10 x 3.5 cm, there was concern preoperatively about the need to make a significant incision in the abdomen for specimen extraction. After the initial laparoscopic splenectomy through the transabdominal approach, the specimen was placed in an endocatch bag and left in the upper abdomen. Laparoscopic vaginal hysterectomy was then done. Prior to the closing of the vaginal cuff, with persistent gentle manipulation, the spleen was extracted through the vagina without any architectural distortion. The vaginal cuff was then repaired in a routine manner. This avoided a large incision in the abdomen. Estimated blood loss was 150 ml. The spleen weighed 425 grams. Patient recovered well from the surgery.
Conclusions
Use of natural orifice for solid tumor extractions may be feasible in selected patients without oncological compromise. Laparoscopic resections for massive splenomegaly, although challenging, can be safely accomplished even in a community setting. Concomitant laparoscopic gynecologic and general surgery procedures can be done with good functional outcomes.
Keywords
Laparoscopy; Natural Orifice; Splenectomy; Vaginal Hysterectomy
Background
The introduction of laparoscopy has revolutionized abdominal surgery offering a minimal invasive approach for various procedures with significantly reduced postoperative complications. In the meantime laparoscopic procedures have found broad acceptance in oncologic surgery especially for the staging of gastrointestinal cancer and colorectal resections [1-3]. However, one of the limitations of laparoscopic solid organ surgeries is making a relatively big incision for specimen extraction. This is often encountered with large tumors and in cases where morcellation of the specimen would distort the tissue architecture hindering pathological examination.
A recent development is the application of natural orifice transluminal endoscopic surgery (NOTES) using transgastric, transcolonic, transvesical or transvaginal access pathways for a variety of surgical interventions [4]. There are a number of potential benefits to using NOTES over traditional surgical techniques that such as the lack of surface incision including the elimination of surgical site infections and any visible scarring; a reduction in pain, the need for anesthesia, analgesia, recovery time, hernia formation and adhesions; and the ability to perform procedures in patients where an abdominal incision is not feasible, such as in the morbidly obese [5-8].
Transvaginal extraction of the resected intraabdominal viscera, including the spleen, was described in the early 1990s, but the technique was not widely adopted. NOTES has been used for transgastric splenectomy in the experimental setting, but there is no information about the application of NOTES or hybrid NOTES in the management of the spleen in humans [9]. This study highlights the use of a natural orifice for specimen extraction to avoid the limitations associated with laparoscopic solid organ surgeries.
Case Presentation
A 34 year old female with a history of Hodgkin’s Lymphoma and dysfunctional uterine bleeding presented with a new splenic lesion. The patient previously suffered from itching, night sweats, fever, weight loss and severe fatigue. She was found to be anemic. The patient previously received a chemotherapy regimen of Adriamycin, Bleomycin, Vinblastine and Dacarbazine (ABVD). The patient had a history of menometrorrhagia, as well as multiple problems with ovarian cysts. Her past surgical history was significant for bilateral tubal ligation. The patient did not desire to maintain fertility.
A CT scan was performed of the abdomen and pelvis with and without intravenous contrast showing a 5 x 4 cm heterogeneous mass in the spleen as displayed in Figure 1.
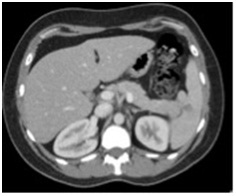
Figure 1: CT scan of the abdomen showing a 5 x 4 cm heterogeneous mass in the spleen
A concomitant laparoscopic splenectomy for massive splenomegaly and laparoscopic-assisted vaginal hysterectomy and bilateral salpingo-oophorectomy for menometrorrhagia was performed under general anesthesia. Given the significant size of the specimen there was concern preoperatively about the need to make a significant incision in the abdomen for specimen extraction.
The patient was prepped and draped in right lateral decubitus position over a beanbag for the laparoscopic splenectomy. Initially, a 10 mm Hassan trocar was placed in the supraumbilical portion using a vertical midline incision. Then, under direct visualization, an additional 12 mm port was placed in the left upper quadrant, and two 5 mm ports were placed in the left subcostal region.
Mobilization of the splenic flexure of the colon was performed using the Harmonic scalpel. Then, the short gastric vessels were divided. A portion of the omentum that was adherent to the anterior medial portion of the spleen was also divided with the Harmonic scalpel. The spleen was mobilized. The splenic hilar vessels were taken down with a Covidien stapler. An Endocatch bag was placed in the abdomen and the spleen was placed within the Endocatch bag and left inside the abdomen with a long suture attached, placed close to the pelvis.
The patient was then repositioned in the dorsal lithotomy position and re-prepped and re-draped to undergo laparoscopic-assisted vaginal hysterectomy and bilateral salpingo-oophorectomy.
The posterior peritoneum was entered and the uterus, ovary, and fallopian tube were delivered. Then, with persistent gentle manipulation, by pulling the suture attached to the Endocatch bag, the spleen and the Endocath bag were brought down to the vaginal opening and the spleen was delivered through the vagina intact as shown in Figure 2.

Figure 2: The spleen and the Endocatch bag being pulled through the vaginal opening
The vagina was closed with interrupted figure-of-eight sutures of 0 Vicryl encompassing the anterior and posterior peritoneum. The vagina was irrigated with copious amounts of sterile saline and bacitracin solution.
The abdomen was inspected for hemostasis and irrigated copiously with sterile saline and antibiotic solution. The operation was the completed by placing a Blake drain through the left lateral port site. This was sutured in place. The 15 mm and 12 mm port sites were closed with the endoplication device and the umbilical port was closed under direct visualization utilizing 0 Vicryl sutures. The patient's anesthesia was reversed and she was taken to the recovery room in a stable condition.
This method avoided a large incision in the abdomen. The estimated blood loss was 150 ml. The spleen weighed 425 grams, and measured 17 x 10 x 3.5 cm as shown in Figure 3.
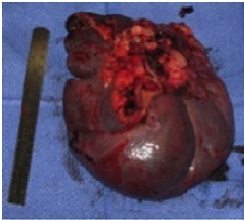
Figure 3: The extracted spleen measured 17 x 10 x 3.5 cm and weighed 425 grams
Pathology showed multiple tumor nodules with sheets of large atypical cells in a background of neutrophils, eosinophils, lymphocytes and plasma cells as shown in Figure 4.
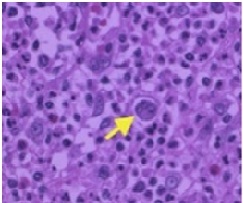
Figure 4: Histopathology
By immunohistochemistry, the large cells were determined to be positive for CD15, CD30 and negative for CD20 and CD45. CD3 highlights the small T-cells and CD20 highlights the small B-cells in the background. These features were consistent with splenic involvement by classical Hodgkin lymphoma. The margins were free of disease.
There were no complications during the procedure, and the patient recovered well from the surgery. The patient was discharged to home at day nine following surgery.
Discussion
Natural orifice specimen extraction using either the vagina or anus as a route eliminates the need for abdominal wall incision for specimen extraction and anastomosis construction. The natural orifice specimen extraction concept is appealing as it maximizes the benefits of laparoscopic surgery while reducing potential wound complications, and provides experience for cautious progression toward incision-less surgery. Smaller incisions not only improve the cosmetic results but also decrease postoperative pain, which is directly associated with incision length [10].
One criticism of the laparoscopic approach has been the lack of tactile feedback and perhaps an inability to identify accessory splenic tissue. The incidence of accessory spleen is approximately 15% [11]. Failure to detect and remove accessory splenic tissue may lead to treatment failure in case of malignancy. Studies show that the lack of the ability to palpate does not compromise the surgeon's ability to find and remove accessory splenic tissue when laparoscopic splenectomy is compared to open splenectomy [12,13].
Vaginal specimen extraction has been well established in the gynecologic literature. For patients with ovarian, endometrial, or cervical cancer, laparoscopic resection and surgical staging have been performed using vaginal specimen extraction with no compromise of oncologic or functional outcomes [14-16]. Moreover, the rate of dyspareunia is not reported to be significant after posterior colpotomy and specimen retrieval [17,18].
Conclusions
We acknowledge that the implications of this case report are limited because transvaginal extraction of large intraabdominal specimens would be feasible only if a vaginal hysterectomy is concomitantly performed. Nevertheless, we demonstrate that the use of natural orifice for solid tumor extractions may be feasible in selected patients without oncological compromise. Laparoscopic resections for massive splenomegaly although challenging, can be safely accomplished even in a community setting. Concomitant laparoscopic gynecologic and general surgery procedures can be done with good functional outcomes.
Ethical Considerations
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing Interests
The authors declare that they have no competing interests.
Authors’ Contributions
SM participated in concept, data collection and writing. BP participated in data collection and writing. DG, CS and SW participated in writing and critical revision. CS participated in concept, writing and critical revision. All authors read and approved the final manuscript.
Acknowledgments
This study was funded by Cancer Treatment Centers of Americaâ.
References
[1]Hunerbein M, Rau B, Hohenberger P, Schlag PM: The role of staging laparoscopy for multimodal therapy of gastrointestinal cancer. Surg Endosc 1998, 12:921-925.[pubmed]
[2]Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, Pique JM: The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 2008, 248:1-7.[pubmed]
[3]Whelan RL: Laparotomy, laparoscopy, cancer, and beyond. Surg Endosc 2001, 15:110-115.[pubmed]
[4]Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV: Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc 2004, 60:114-117.[pubmed]
[5]Baron TH: Natural orifice transluminal endoscopic surgery. Br J Surg 2007, 94:1-2.[pubmed]
[6]Giday SA, Kantsevoy SV, Kalloo AN: Principle and history of Natural Orifice Translumenal Endoscopic Surgery (NOTES). Minim Invasive Ther Allied Technol 2006, 15:373-377.[pubmed]
[7]Hochberger J, Lamade W: Transgastric surgery in the abdomen: the dawn of a new era? Gastrointest Endosc 2005, 62:293-296.[pubmed]
[8]McGee MF, Rosen MJ, Marks J, Onders RP, Chak A, Faulx A, Chen VK, Ponsky J: A primer on natural orifice transluminal endoscopic surgery: building a new paradigm. Surg Innov 2006, 13:86-93.[pubmed]
[9]Targarona EM, Gomez C, Rovira R, Pernas JC, Balague C, Guarner-Argente C, Sainz S, Trias M: NOTES-assisted transvaginal splenectomy: the next step in the minimally invasive approach to the spleen. Surg Innov 2009, 16:218-222[pubmed].[pubmed]
[10]Truong T, Arnaoutakis D, Awad ZT: Laparoscopic hybrid NOTES liver resection for metastatic colorectal cancer. Surg Laparosc Endosc Percutan Tech 2012, 22:e5-e7.[pubmed]
[11]. Rudowski WJ: Accessory spleens: clinical significance with particular reference to the recurrence of idiopathic thrombocytopenic purpura. World J Surg 1985, 9:422-430.
[12]Franciosi C, Caprotti R, Romano F, Porta G, Real G, Colombo G, Uggeri F: Laparoscopic versus open splenectomy: a comparative study. Surg Laparosc Endosc Percutan Tech 2000, 10:291-295.[pubmed]
[13]Sampath S, Meneghetti AT, MacFarlane JK, Nguyen NH, Benny WB, Panton ON: An 18-year review of open and laparoscopic splenectomy for idiopathic thrombocytopenic purpura. Am J Surg 2007, 193:580-583 [pubmed]
[14]Jung US, Lee JH, Kyung MS, Choi JS: Feasibility and efficacy of laparoscopic management of ovarian cancer. J Obstet Gynaecol Res 2009, 35:113-118.[pubmed]
[15]Malzoni M, Tinelli R, Cosentino F, Fusco A, Malzoni C: Total laparoscopic radical hysterectomy versus abdominal radical hysterectomy with lymphadenectomy in patients with early cervical cancer: our experience. Ann Surg Oncol 2009, 16:1316-1323.[pubmed]
[16]Wong CK, Wong YH, Lo LS, Tai CM, Ng TK: Laparoscopy compared with laparotomy for the surgical staging of endometrial carcinoma. J Obstet Gynaecol Res 2005, 31:286-290.
[17]Ghezzi F, Raio L, Mueller MD, Gyr T, Buttarelli M, Franchi M: Vaginal extraction of pelvic masses following operative laparoscopy. Surg Endosc 2002, 16:1691-1696.
[18]Yoong W, Pillai R: Posterior colpotomy-a retrieval route for solid ovarian tumours. BJOG 2009, 116:465-466. [pubmed]


