Case Report

Multimodal Treatment for Undiferentiated Carcinoma of the Lacrimal Sac
1Hiroshi Doi, 1Masayuki Fujiwara, 1Yasuhiro Takada,1Yasue Niwa, 1Norihiko Kamikonya, 2Maki Tonooka, 3Takashi Ito, 4Tomonori Terada, 2Masao Kakibuchi, 1Shozo Hirota
- 1Department of Radiology, Hyogo College of Medicine, 1-1, Mukogawa-cho, Nishinomiya City, Hyogo, Japan.
- 2Department of Plastic Surgery, Hyogo College of Medicine, 1-1, Mukogawa-cho, Nishinomiya City, Hyogo, Japan.
- 3Department of Surgical Pathology, Hyogo College of Medicine, 1-1, Mukogawa-cho, Nishinomiya City, Hyogo, Japan.
- 4Department of Otolaryngology, Hyogo College of Medicine, 1-1, Mukogawa-cho, Nishinomiya City, Hyogo, Japan.
- Submitted: August 6, 2012
- Accepted : September 8, 2012
- Published: October 8, 2012
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction
Primary undifferentiated carcinomas of the lacrimal sac are extremely rare with only a few documented cases and with no cases of Japanese patients to best of our knowledge.
Case report
A 49-year-old female with lacrimation and an orbital mass was referred to our hospital. FDG-PET did not reveal any evidence of metastatic diseases. The patient was treated with a wide resection of right orbital tumor. The pathological examination led to a diagnosis of undifferentiated carcinoma. The postoperative site received 60 Gy in 30 fractions as adjuvant radiotherapy. Neck dissection was performed later. Two cycles of systemic chemotherapy, consisting of docetaxel, cisplatin, and 5-fluorouracil, were delivered sequentially. However, multiple metastatic lesions occurred in the lung, skin and lymph nodes. The patient died 7 months after the initial operation.
Conclusion
The undifferentiated carcinoma of the lacrimal sac exhibited an aggressive behavior with a poor prognosis. Therefore, a careful follow-up is required, because recurrence and metastasis may occur within a very short period of time after the initial treatment.
keywords
Lacrimal sac tumor, Orbital tumor, Undifferentiated carcinoma, Radiotherapy, Head and neck cancer
Introduction
Almost 400 lacrimal sac tumors have been reported [1].Most lacrimal sac tumors are misdiagnosed as dacryocystitis and lacrimal sac obstructions. Whereas, 55 to 72 % of the lacrimal sac tumors were reported to be malignant, and the reported mortality rate ranges from 37.5 to 50% [1-5].In addition, squamous cell carcinoma and transitional cell carcinoma seem to be common [2].However, primary undifferentiated carcinomas of the lacrimal sac are extremely rare with only a few documented cases and with no cases of Japanese patients to best of our knowledge [2,6,7].The report presents a case of undifferentiated lacrimal sac carcinoma that was treated by surgery, radiotherapy and chemotherapy.
Case Report
A 49- year-old female was referred with a diagnosis of a right orbital mass. She had no significant medical history. Magnetic resonance imaging (MRI) was performed following one month history of treatment for inveterate dacryocystitis with lacrimation and an orbital mass. MRI revealed a heterogeneously enhanced mass in the inner orbit (Figure 1-A,B).The specimen from the initial biopsy yielded a pathological diagnosis of sebaceous carcinoma.
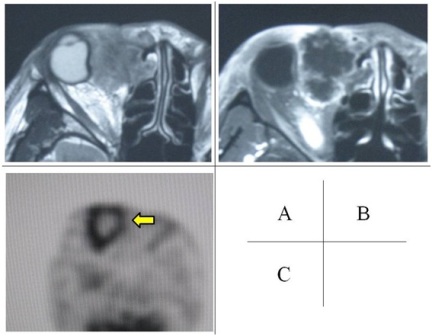
Figure 1: Mass in the inner orbit on MRI imaging and on FDG-PET/CT imaging. An ill-defined mass existed in the inner orbit. Axial T2-weighted image showed nonspecific heterogeneous intermediate intensity of right lacrimal sac with unclear margin (A). Axial post gadolinium T1-weighted image showed a peripheral margin of increased signal (B).FDG-PET/CT images showed increased uptake of FDG in the peripheral areas of the mass (arrow). The blood glucose level was 238 mg/dl in the PET/CT scanning (C).
The results of laboratory tests were nonspecific abnormal results except for the blood glucose level of 249 mg/dl.
18F-2-fluoro-2-deoxyglucose (FDG) positron emission tomography (PET) combined with computed tomography (CT) revealed no evidence of either metastatic diseases or any lymphadenopathy (Figure 1-C).Non-contrast enhanced CT revealed invasion of the ethmoid sinus with osteolytic changes in the inner orbit.
She underwent a radical operation for the right orbital tumor on the 50th day after the initial MRI. The operation included a wide resection of the tumor, orbital exenteration, partial excision of the maxilla, excision of the ethmoid sinus, and reconstruction surgery with a rectus abdominis musculocutaneous flap.
The mass measured 47 x 44 mm and it was found to have displaced the right ocular globe laterally. The pathological findings are shown in (Figure 2).The pathological findings suggested an undifferentiated tumor with highly invasive behavior. However, the surgical margins were tumor free.
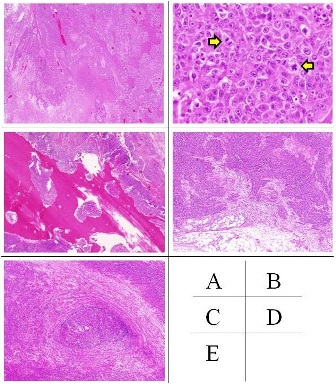
Figure 2: Pathological findings (Hematoxylin-eosin (HE) staining (A)(B)(C)(D), Victoria blue and HE compound staining (E)The pathological examination revealed no evidence of any differentiation, unclear origin of the cells, and the tumor was diagnosed as undifferentiated carcinoma of right lacrimal sac (A; HE staining, original magnification x12.5). An intermediate to high mitotic activity was recognized. (arrows, B; HE staining, original magnification x400). The tumor consisted of infiltrating bone, fat, and vessels, but was separated from the eye globe (C; HE staining, original magnification x20, D; HE staining, original magnification x20, E; Victoria blue and HE compound staining, original magnification x40). There was no evidence of ocular invasion.
The patient underwent 60 Gy of postoperative radiotherapy which was delivered in 30 fractions with 4 MV X-rays. The dose distribution of radiotherapy is shown in (Figure 3). Subaural lymphatic metastasis was found in CT during the treatment period of radiotherapy. Therefore, right neck dissection was performed. Nodal metastases of undifferentiated carcinoma were found in the subaural lymph nodes, parotid lymph nodes and submandibular lymph nodes.
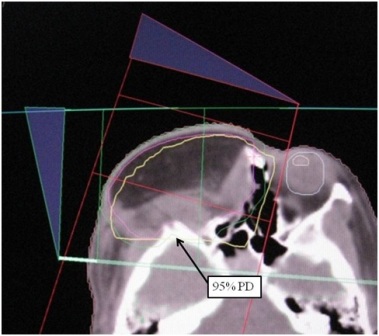
Figure 3: Dose distribution of postoperative radiotherapy The solid line of postoperative site shows a 95% prescribed isodose line (arrow). The line well covered the postoperative site where the tumor had been resected.
FDG-PET/CT revealed the FDG uptake in the left upper deep cervical lymph node and small nodules in the right inferior lobe of lung at the end of radiotherapy. Further, contrast enhanced CT image revealed metastatic tumors of right parotid gland. Extirpation of the metastatic tumors of the right parotid gland was performed one and half months after radiotherapy.
Then, the patient was treated with chemotherapy. The regimen of chemotherapy (TPF) was 60 mg per square meter docetaxel (TXT), 60 mg per square meter cisplatin (CDDP), and 5000 mg per body 5-fluorouracil (5-FU) in 5 days. The same regimen of chemotherapy was administered 4 weeks later. CT after chemotherapy showed that the size of the lung nodules increased, carcinomatous lymphangiosis was suspected and mediastinal lymphadenopathy was found. In addition, skin metastasis was found to occur in the anterior neck. TS-1 was delivered as the second-line chemotherapy. Skin metastasis progressed with the appearance of multiple skin metastases, and lung metastases also progressed, although no evidence of local recurrence was observed, in non-contrast CT after the administration of TS-1. The patient’s general status thereafter continued to gradually worsen and she died 7 months after the initial operation.
Discussion
Primary undifferentiated carcinoma-high-grade malignant tumors of the lacrimal sac are extremely rare, and have been so far reported in a 55-year-old male, age 72-year-old female, age 94-year-old female, and 49-year-old female (the present case) [2,6,7]. The traditional treatment of suspected lacrimal sac tumors includes radical resection, RT, or chemotherapy. Ni, et al., reported wide excision combined with radiotherapy at 30 to 50 Gy decreased the rated of recurrence [4].In addition, Low, et al., reported a favorable outcome of undifferentiated carcinoma of the lacrimal sac after treatment included postoperative radiotherapy at a dose of 66 Gy using the method of intensity modulated radiotherapy [6]. The current case was treated with postoperative radiotherapy of 60 Gy using 3-dimensional conformal radiation therapy. No apparent locoregional failures were observed, although skin metastasis appeared in the marginal zone of the field of radiotherapy. TPF is considered as one of the standard regimes of chemotherapy for advanced head and neck cancer [8]. However, the benefit was limited in the current case.
Conclusion
Primary undifferentiated carcinoma of the lacrimal sac is extremely rare and exhibits aggressive behavior with a poor prognosis. Therefore, it requires a careful follow-up. In addition, the treatment strategies and effective management regimes for undifferentiated carcinomas should therefore be investigated in order to identify an optimal treat protocol.
Authors' Contribution
HD: Designed and conceived the study, reviewed the literatures and prepared of draft manuscript.
MF: Supervised radiotherapy.
YT: Supervised radiotherapy.
YN: Edited the manuscript.
NK: Concept and design, supervised radiotherapy, edited the manuscript, and supervised the article.
MT: Performed surgical procedure.
TI: Examined surgical specimen, wrote pathological report and provided histological photographic slides
TT: Performed surgical procedure and chemotherapy
MK: Performed surgical procedure and supervised final revision of the article
SH: Supervised final revision of the article
All authors read and approved the final manuscript.
Conflict of Interests
The authors declare that they have no conflict of interest.
Ethical Considerations
Written informed consent was obtained from the patient for publication of this case report.
References
[1]. Heindl LM, Junemann AG, Kruse FE, Holbach LM. Tumors of the lacrimal drainage system. Orbit. 2010;29:298-306.[Pubmed]
[2]. Stefanyszyn MA, Hidayat AA, Pe'er JJ, Flanagan JC. Lacrimal sac tumors. Ophthal Plast Reconstr Surg. 1994;10:169-184.[Pubmed]
[3]. Spaeth EB. Carcinoma in the region of the lacrimal sac. Arch. Ophthalmol.1957;57:689-693. [Pubmed]
[4]. Ni C, D'Amico DJ, Fan CQ, Kuo PK. Tumors of the lacrimal sac: a clinicopathological analysis of 82 cases. Int Ophthalmol Clin. 1982;22:121-140.[Pubmed]
[5]. Montalban A, Liétin B, Louvrier C, et al. Malignant lacrimal sac tumors.Eur Ann Otorhinolaryngol Head Neck Dis. 2010;127:165-172.[Pubmed]
[6]. Low JR, Bian Ng S, Sundar G. Undifferentiated carcinoma of the lacrimal sac: case report and review of literature. Orbit. 2011;30:293-296.[Pubmed]
[7]. Parmar DN, Rose GE. Management of lacrimal sac tumours. Eye (Lond). 2003;17:599-606.[Pubmed]
[8]. Vermorken JB, Remenar E, van Herpen C, et al. Cisplatin, fluorouracil, and docetaxel in unresectable head and neck cancer.N Engl J Med. 2007; 25;357:1695-1704.[Pubmed]


