Review

Psychosocial Interventions for Cancer Patients and Outcomes Related to Religion or Spirituality: A Systematic Review and Meta-Analysis
1,Matthew Goldenberg2Anne Moyer* 2Stefan Schneider, 3, Stephanie J. Sohl 4Sarah Knapp
- 1George Mason University, Graduate School of Education, 4400 University Drive MS4D1
- 2Department of Psychology, Stony Brook University
- 3Applied Behavioral Medicine Research Institute, Vanderbilt University Medical Center Twelfth Floor, Suite 1200
- 4Southern Vermont College, 982 Mansion Drive
- Submitted:Sunday, April 13, 2014
- Accepted:Thursday, May 01, 2014
- Published:Friday, May 09, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
Religion and spirituality areimportant aspects of life for many individuals
and have been shown to be potentially useful in therapy. This hold relevance to patients coping with cancer.
Study Design
In this systematic andmeta-analytic review, we examined the extent to which psychosocial interventions for cancer patients improve spiritual or religious quality of life.
Materials and Methods
We drew reports from a database of 932 unique projects that evaluated the effectiveness of psychosocial interventions for cancer patients reported over three decades. We identified 78 projects that measured religious or spiritual outcomes for inclusion in the current review. We investigated the types of interventions that these comprised, the types of spiritual or religious outcomes assessed. For 20 studies for which data were available we calculated effect sizes for religious or spiritual quality of life and examined the potential moderating roles ofpatient genderand race/ethnicity on the interventions’ effects.
Results
We found that overall psychosocial interventions were beneficial for cancer patients’ religious or spiritual quality of life (d = .29), but did not find any moderating effects.
Conclusions
Psychosocial interventions have small but significant effects on outcomes related to religion or spirituality. Yoga, meaning-centered therapy, and life review therapy may be particularly useful interventions for cancer patients for improving outcomes in these important domains.
Key Words
Neoplasms, therapy, quality of life
Introduction
Religion and spirituality have a central place in life for many individuals, with telephone surveys documenting that 83% of Americans believe that religion is either very important or fairly important in their lives, that 91% believe in God or a universal spirit, and that 83% identify with some form of religion [1,3]. Religious and spiritual elements can also be an important part of therapeutic interventions,althoughthis depends on the preferences of the client and provider[4]. Theawareness of different religious beliefs and valuesis part of the American Psychological Association’s definition of multicultural competence for therapists[5] and this competence is associated with higher client ratings of therapists’ empathy, the quality of their working alliance, and satisfaction with therapy [6].Religious individuals prefer religiously similar counselors and choose to discuss more intimate topics with them[7,8].
Religion and spirituality have also been shown to play important roles in coping with cancer diagnosis and treatment[9,15].Religion and spirituality may be particularly important elements of therapeutic interventions for cancer patients because the disease often evokes existential themes of control, identity, relationships with others, and meaning [16,17]. Psychosocial interventions may help patients work through tensions between the meaning they attribute to cancer and their beliefs about a higher power[18] or their acceptance of a difficult situation [19]. Religious affiliation may also play a role in coping with illness. For example, Seventh Day Adventists may experience more distress over illnesses because the emphasis on maintaining one’s body’s health [20]. Religious affiliation may influence the efficacy of particular psychosocial interventions. Because the Jewish tradition focuses on knowledge, emotional expression, and understanding inner emotions, talking or insight-oriented therapies may resonate more with Jewish individuals[21].
Although religion and spirituality have relevance to healing, the influence of religion on health and mental health is an understudied topic. For example, in a review of publications in seven major American Psychological Association journals from 1991 to 1994, only 2.7% included a religion-oriented variable, and in a majority of these (79%) the religion-oriented measure only involveda single item[22]. In a review of four major psychiatric journals, just 2.5% of studies including a religion-orientedvariable [23]. Furthermore, a focus on the Christian faithdominates the limited research on religion and health [24]and researchers that study religion havefocused on theistic religions at the exclusion of agnostic or atheist belief systems[25,26]. Despite the potential importance of religion and spirituality for cancer patients, no reviewhas systematically examinedthe research on the ways in whichpsychosocial interventions for cancer patients designed to improve quality of lifemay affect outcomes related to religion or spirituality. Relatedreviews have focused on religious coping and psychological adjustment to stress [27], intercessory prayer [28,30], spiritual needs in health care settings [31], religion and psychotherapy [8], religion or spirituality and mental health [32,33], religious attendance and health [34], spirituality and end of life care [35], religious involvement and mortality [36], psychotherapeutic practices and religion [37], and religion and spirituality’s relationship to breast cancer patients quality of life [38].
In sum, religion and spirituality hold a central place for many individuals, are potentially usefulin therapy, and arerelevant to patients coping with cancer. In our prior systematic review work[39,40], we generated a database of 932 unique projects that evaluated the effectiveness of psychosocial interventions designed to improve several aspects of quality of life for cancer patients reported over three decades. In the current systematic andmeta-analytic review, we used this database to examine the extent to which such psychosocial interventions for cancer patients improvespiritual or religious quality of life specifically. Furthermore, we sought to describe the types of interventions that these comprise andthe types of spiritual or religious outcomes assessed.
We also aimed toexamine the potential moderating roles ofgenderand race/ethnicity on these effects.Religion and spiritualityhave been shown to be particularly important for women[1,41,43] and various elements of religion appear to affect the health of men and women differently [44,46]. In the context of cancer, a survey of older Whitelung cancer patients showed that women were more likely than men to favor spiritual practices, use religious coping, endorse having a life mission, and feel that they were part of a divine plan [47].Religion and spirituality have also been shown to beparticularlyrelevant for African Americans[1,48,49] and their physical [43] mental health [50,51] and possibly to coping with cancer.
In our review, we did not differentiate between religion and spirituality due to the significant overlap between these two concepts [28,52]. We included projects that looked at existential quality of life because some authors have defined this as a sub-construct of religion or spirituality [53,54]. We hypothesized that psychosocial interventions would have a beneficial effect on the religious or spiritual quality of life in cancer patients. Additionally, because of the importance women and African Americans place on religion and spirituality, we expected that studies that included a larger proportion of women and African Americans in their samples mightshow stronger effects.
Method
Study Identification for the Larger Database
Studies included in the database examined psychosocial interventionsfor adult cancer patients that: (1) reported outcomes on psychological,emotional, behavioral, physiological, functional, ormedical status; (2) were first reported as a published article oran unpublished dissertation between January 1980 and December 2010; and (3) included 10 or more individuals per group. Electronic databases (PsycINFO,PubMed, and Dissertation Abstracts International) weresearched using key terms (e.g.,cancer, neoplasms, tumor, and psychosocialintervention, psychotherapy, psychological treatment,education, cognitive behavioral, relaxation, stress management,support group, self-help group, nursing intervention, biofeedback;a full list is available from the authors upon request). The referencelists of included reports and of 146 prior reviews and meta-analysesalso were examined. Descendancy searches were conducted onprior reviews (i.e., for subsequent studies citing them), and tablesof contents of several journals (e.g., Psycho-Oncology, Journal of ClinicalOncology, Cancer) were searched.The sample included 932 reports. Separate reports based on the same sample(e.g., separate studies reporting outcomes at 3-month and 12-month follow-up) were treatedas a single project.
Project Eligibility for the Current Review
Projects eligible for this review were those in the database that included a religious- or spirituality-related outcome. Because one goal was to describe the content and scope of this literature broadly in addition to summarizing findings quantitatively, we included any article that assessed this type of outcome regardless of whether or not results were reported in a way that allowed us to calculate an effect size. We subjectedthe subset of studies for which an effect size could be calculated to statistical meta-analysis. Religious- or spirituality-relatedoutcome measures were those that were identified as such in the title of the assessment instrument (e.g., Functional Assessment of Chronic Illness Therapy-Spiritual Well Being, FACIT-Sp), regardless of whether the full instrument, or a portion thereof, was used.Projects alsowere eligible if they included any outcome measure that made reference to having a connection to a higher power,existential quality of life, or religious institutional beliefs or practices (e.g., prayer, reading the bible).
Project Abstracting
We abstracted from each project: the types of religion and spirituality outcomes measured, a description of the type of intervention(s) delivered, and, participants’ gender, race/ethnicity, and religion
Data Analysis
For a study to be included in the meta-analytic syntheses, sufficient data to calculate individual effect sizes for religion and spirituality outcomesneeded to be presented. In calculating aggregate effect sizes, we included onlystudies that used the complete religious or spiritual quality of life measure. We also did not include studies that combined spiritual or religious quality of life with other types of quality of life.If a study compared two active interventions we randomly selected one of these to include in the aggregate effect size analysis to preserve the independence of study effect sizes.
Prior to aggregating study effect sizes, we screened for potential outliers that were two or more standard deviations away from the mean and ran sensitivity analyses with and without these outliers.We ran separatemixed-effect meta-regressions (method of moments) using thetwopotential moderator variables gender (percentage of the sample that was female)andrace/ethnicity(percentage of sample that was African American) for the subset of studies that reported these.
Results
We identified 78studiesfor this review. The majority of studiesincluded samples that were predominantly female (86%) and White (83%). Many studies (38%), however, did not report the race/ethnicity of their participants and a substantial proportion did not report their religious affiliation (77%). Where this was reported, 13 studies included a mostly Christian population and two studies recorded only on the presence or absence of religion or religious practice.
Table 1 highlights details of the variety of activities and techniques comprising representative interventions (i.e., group therapy, meaning-centered therapy, psychoeducational therapy, mindfulness therapy) used in studies that assessed religious or spiritual outcomes. These included education about religious issues, yoga, meditation, reflecting on life, imagery exercises, support groups, art therapy, cognitive restructuring, exercising, tai chi, music therapy, and counseling.
Table-1:
Representative Interventions
| Group Therapy |
Lifestyle change and group support program with the emphasis on psychospiritual issues and inner process. Health series discussion group: information on nutrition and exercise. Dance/movement group: yoga, dance therapy, experiential work with silent meditation, experiential work with imagery, and writing and drawing exercises. Discussion group: emphasis on support. |
| Meaning-Centered Therapy |
Utilizes didactics, discussion, and experiential exercises that focus around themes related to meaning and advanced cancer. (e.g., Session 3: addresses the historical context of meaning. Patients are asked to reflect on their life and identify the most significant memories, relationships, and traditions that have made the greatest impact on them. Session 5: explores attitudinal sources of meaning. Patients participated in an experiential exercise wherethey are asked to respond to questionslike "What would you consider a good or meaningful death?") |
| Psychoeducational Therapy |
Session 1 = addresses physical well-being, pain, lymphedema, and cancer-related fatigue. Session 2 = addresses psychological well-being, social well-being, menopausal symptoms, emotions, family, financial, and social relationships, and health maintenance. Session 3 = addresses spiritual well being, hope, meaning in illness, uncertainty over the future, and spirituality. |
| Mindfulness Therapy |
Guides participants to achieve greater awareness of themselves, their thoughts, and their bodies through class discussion, meditation, and yoga. |
Table 2 shows thebroad types of
religious and spiritual outcomes assessed. The most commonly assessed were
spiritual or religious quality of life (53%) and spiritual and religious coping
(21%). Less commonly assessed types included posttraumatic growth, existential
quality of life, locus of control, hope, forgiveness, and the extent to which
cancer interferes with a patient’s standard life activities. A small subset of
studies (6%) assessed outcomes qualitatively.In terms of specific instruments,
the FACIT-Sp [55]was commonly used to measure spiritual quality of life(23/41
studies) while the Brief RCOPE [56]and the Trier Coping with Illness
Scale[57]were commonly used to assess religious coping (3/16 and 3/16 studies,
respectively). There was substantial variability in how religious coping was
assessed, however. These measures included counts of the number of people who
used a particular coping method (3 studies), tallies of the use of particular
religious coping strategies (e.g., prayer [11 studies], the extent to which a
patient endorsed a particular statement [1 study], and measures that considered
both positive and negative forms of religious coping [1 study]). The 11 studies
that tallied the use of religious coping strategies can be further categorized
into measures that focused on the total use of particular coping strategies like
prayer (2 studies), measures that measured religious coping with just one item
(3 studies), and measures that focused on constructs (e.g., search for religious
meaning) peripheral to specific types of religious coping like prayer (6
studies).To highlight the operational definitions of religious and spiritual
outcomes, Table 3 provides descriptions of a subset of the measures that assessed the most common types of outcomes presented in these studies.
Table 2: Types of Religious or Spiritual Outcomes Assessed
|
|
Number (%) of Studies
|
|
Religious or Spiritual Quality of Life
|
41 (53%)
|
|
Religious or Spiritual Coping
|
16 (21%)
|
|
Post Traumatic Growth
|
5 (6%)
|
|
Existential Quality of Life
|
5 (6%)
|
|
Qualitatively Assessed Outcomes
|
5 (6%)
|
|
Locus of Control
|
3 (4%)
|
|
Hope
|
2 (3%)
|
|
Forgiveness
|
1 (1%)
|
|
Interference with Life Activities
|
1 (1%)
|
Table-3: Representative of Types of Religious and Spirituality Outcome Measures Assessed
|
Quality of Life
|
FACIT-SP
|
This is a self-report
measure of quality of life designed for cancer patients. It has 28 items
designed to assess 7 domains common to all cancer patients. It measures
meaning and purpose, harmony and peace, and closeness to God or a higher
power. It is divided into two subscales, faith/spiritual beliefs and
meaning/peace. It has a Cronbach’s alpha of .87 (Peterman et al., 2002).
|
|
Coping
|
The Brief COPE
|
The Brief COPE is a
28-item inventory. It contains scales for adaptive and maladaptive
coping. Under adaptive coping there is a religious coping question. This
scale is based on a 4-point response format indicating the overall use
of the coping method from 1 (not at all) to 4 (a lot). Cronbach’s alpha
is .81 and .57 for adaptive coping and maladaptive coping, respectively
(Carver, 2007)
|
|
Existential Quality of
Life
|
McGill QOL Scale
|
This is a 16-item
self-report scale that measures quality of life. It has four subscales,
physical, psychological, existential (e.g., “In achieving life’s goals,
I have made no progress whatsoever/progressed to complete fulfillment),
and support. The McGill QOL scale has a Cronbach alpha of >.79 (Cohen et
al., 1995)
|
|
Post Traumatic Growth
|
PTGI-R
|
This is a 21-item
self-report inventory that measures the individual’s perception of
positive changes after a traumatic life experience. An individual rates
from 0-6 the extent to which their views changed as a result of their
illness. There are five
subscale scores and a total score that can be derived from these
subscales. The subscales
are: relation to others; new possibilities; personal strength; spiritual
change, and appreciation for lifef. Cronbach’s alpha was .90.
Test-retest reliability two months later was .71 (Tedeschi & Calhoun,
1996).
|
|
Hope
|
Herth Hope Index
|
This is a 32-item
self-report inventory. This measure delineates three factors in hope:
temporality and future, positive readiness and expectancy, and
interconnectedness. Sample items include: “I have a positive outlook
towards life,” “I believe each day has potential,” and “I am able to
give and receive caring love.” In past studies the measure had a
test-retest reliability of .91 and a Cronbach’s alpha of 0.97 (Hearth,
1992).
|
|
Forgiveness
|
Enright Forgiveness
Inventory
|
This is a 60-item
self-report measure of interpersonal forgiveness towards a person who
has been unfair. It includes 6 subscales (10 items each): positive and
negative affect, positive and negative behavior, and positive and
negative cognition. It ranges from 60-360 with a higher score equal to a
higher level of forgiveness (e.g., “I feel positive towards him or her”
[the offender], “Regarding the person [the offender], I do or would show
friendship” and “I think he or she [the offender] is worthy of
respect.”) Cronbach’s alpha is .90 and above. Test retest-reliability
ranges from .67-.91 (Hansen et al., 2009).
|
Pretest-post test effect sizes were calculated for the largest category of outcome, religious or spiritual quality of life, in active, rather than control, conditions. We did not calculate between-condition effect sizes because, due to the variety of comparison conditions, ranging from wait list control to other types of active interventions, combining these disparate comparisons would be uninformative. Of the 78 studies identified for the review, 41 studies contained information on religious or spiritual quality of life outcomes. In aggregating individual effect sizes for this outcome we excluded 12 studies because they did not provide relevant data to do so, 4 studies because they only used a subscale of the entire spirituality measure, and 5 studies because they combined spiritual or religious aspects of quality of life with other types of quality of life. Additionally, because one article [58] compared two active interventions (Mindfulness Based Stress Reduction and Healing Arts Therapy), we randomly selected the Mindfulness Based Stress Reduction intervention to include in the aggregate effect size. We also chose to include data from two studies that reported adjusted means rather than raw means [59,60]. This resulted in a sample 20 studies to calculate a pretest-post test aggregate effect sizes (N= 861).
In calculating individual study pretest-post test effect sizes, if the test-retest reliability necessary to make this calculation for a particular measure was not reported in the literature, we used .8 as a conservative estimate. This was the case for the majority of the measures assessed, however, a .9 test-retest reliability for the Quality of Life Instrument Breast Cancer Version spirituality subscale was reported [61].
We found the three largest effect sizes in studies that used yoga (d = 1.06;[62]), life review therapy (d= 1.02) [63]), and meaning-centered therapy (d = .72) [64]). The studies investigating yoga and life review therapy were statistical outliers. Pooled random-effect inverse-variance weighted aggregate analyses including these two outliers indicated that psychosocial interventions for cancer patients had a fairly small but significant effect on spiritual or religious quality of life (d = .29, Z = 4.63, p< .001) with a significant amount of heterogeneity(Q(19) = 127.51, p< .001, I = 85.10
(Figure 1). To explain this heterogeneity, we ran separate mixed-effect meta-regressions (method of moments) using the two potential moderators (percentage female and percentage African American).Neither analysis was significant, with or without the outliers.
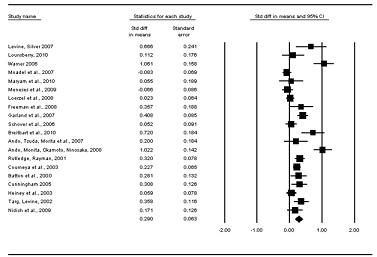
Figure 1.Individual and aggregate effect sizes for religious or spiritual quality of life
Discussion
One goal of our review was to describe the types of psychosocial interventions for cancer patients used in studies that measure religious or spirituality outcomes and to describe the types of these outcomes that have been assessed.We found that interventions used in studies that assess spiritual or religious outcomes were diverse, ranging from simple educational interventions, to interventions focusing on religious or spiritual issues, to mind/body practices such as yoga. We found the three largest effects in studies that used yoga, life review therapy, and meaning-centered therapy.Yoga can facilitate mindfulness and self-compassion [56,65]. Life review therapy may allow patients to reframe their life in a positive way and become more comfortable with death by seeing their life as full, generative, and meaningful [66]. Meaning-centered therapy deals directly with reappraising the role of cancer in a patient’s life. These benevolent appraisals are related to better mental health outcomes [67,68].The most commonly assessed outcome was religious or spiritual quality of life whereas smaller numbers of studies measured religious or spiritual coping, existential quality of life, post traumatic growth, locus of control, forgiveness, hope, and qualitatively assessed religious or spiritual outcomes.For the studies that focused on religious or spiritual quality of life, the FACIT-SP was the most common measure used.For religious coping there was variability in the measures used, with the Trier Coping with Illness Scales and the Brief COPE Survey being the most common.Studies tended to recruit female samples, and of the studies that reported race/ethnicity of their samples a majority of these studies were predominantly White.
We examined the extent to which psychosocial interventions for cancer patients increase cancer patients’ or survivors’ spiritual or religious quality of life and found that,overall, they had a small but significant effect. This effect was not moderated by the gender or race/ethnicity of the samples studied, perhaps due to limited variability in the gender and racial/ethnic make up of samples studied. Thus, these interventions show some promise even though they may not be useful for cancer patients who do not desire a spiritual orientation in their therapy. For patients who do not desire such an orientation, useful elements might include helping them find meaning in their lives, maintaining connection with family and friends, and experiencing and appreciating the natural world[69].
Our observation that a large number of studies included predominantly female samples is similar to what has been observed in the literature on psychosocial interventions for cancer patients as a whole[39] and may reflect a greater amount of federal funding towards breast cancer and ovarian cancer [70,71].Researchers may need to develop and test religious- or spiritually-focused interventions specifically directed at men with cancer. Because feelings of vulnerability are more commonly accepted for women than men[72], future research may need to explore whether or not its beneficial for men to explore vulnerable feelings they may have about God, the afterlife, and death while experiencing cancer. This may be useful in allowing men to express suppressed feelings of fear or anxiety [73].
We found that only a few studies reported the religious affiliation of their participants. Out of those studies that measured religious affiliation, a majority of them used a predominantly Christian population.This is important because it may limit the generalizability of the results to those who identify as Christian.We suggest that future research attend to specific religious orientations when considering the match between therapeutic ingredients and the traditions and beliefs that are involved in a religious faith. However, due to the fact that there are common concepts shared among various faiths [74], it is possible that interventions that are generic in their spiritual offerings, such as those found to be most effective in the current study, will still benefit cancer patients of different religious orientations.We also found that, of the studies that measured race/ethnicity, a majority of the studies studied predominantly White samples. This represents an area for expansion, as cancer patients from minority populations, in particular African Americans, may resonate with spiritually-oriented interventions [50].
The variety of coping measures used in this literature indicates that there is,as yet, little consensus regarding how to measure religious coping in studies examining individuals dealing with cancer. One of the most commonly used measures, the Brief RCOPE, makes an important distinction between positive and negative forms of religious coping that is critical to understanding the effect of psychosocial interventions on a cancer patient’s religious quality of life[51]. This 14-item measure was generated from interviews with people experiencing major life stressors. Positive religious coping (7 items) reflects a secure relationship with a transcendent force and benevolence towards oneself and others. Negative religious coping (7 items) reflects spiritual tensions within oneself, others, and the divine.Positive religious coping is related to stress-related growth,spiritual growth, positive affect, and higher self-esteem, and less depression,anxiety, and distress, whereas negative religious coping is related to more depression, anxiety, and distress [27]. For interventions like mindfulness ([Table 1) that do not attempt to change a patient’s religious coping or view of God, this measure may also provide information on the extent to which a patient’s style of religious coping is related to the influence of an intervention on religious or spiritual quality of life.
The significant, small overall effect size found in this review suggests that psychosocial interventions do improve religious or spiritual quality of life. In addition,meaning-centered therapy, life review therapy, and yoga had the three largest effect sizes among the active treatment conditions studied. These findings are limited in that they are based upon pretest-posttest effect sizes rather than comparisons of active conditions with control conditions. In addition, we were not able to analyze the distinction between positive and negative religious coping.
The lack of support for our hypothesis that there would be a positive relationship between the number of African Americans in a study and the study’s effect on spiritual or religious quality of life,may be due to the limited number of African Americans included in the current literature. More interventions targeted specifically towards African American populations are needed for more conclusive results. Future work could also consider whether practical needs (e.g., money) or spiritual needs (e.g., a church community) play a greater role in the mental health, specifically the religious or spiritual quality of life of an African American with cancer.The lower socio-economic status of African American populations may not influence their religious or spiritual quality of life.
Conclusions
In conclusion,our review highlights that psychosocial interventions for cancer patients do influence religious and spiritual quality of life. However, the existing research is not available to unequivocally determine whether race/ethnicity or gender plays a role in this relationship. Thus, there is a need for research that further explores the possible differential effect of psychosocial interventions on religious and spiritual quality of life in more diverse populations (i.e., racial/ethnic minorities, individuals of diverse religious affiliations, men). Despite the many psychosocial interventions that we identified in the cancer literature as a whole, more work is necessary to understand how to design these interventions to optimally benefit different populations for the purposes of improving religious or spiritual quality of life.
Learning points
Interventions used in studies that assessed spiritual or religious outcomes were diverse, ranging from simple educational interventions, to interventions focusing on religious or spiritual issues, to mind/body practices such as yoga.Psychosocial interventions for cancer patients influenced religious and spiritual quality of life, with their effects being small but significant.Yoga, meaning-centered therapy, and life review therapy may be particularly useful interventions for cancer patients for improving outcomes in these important domains.
Competing interests and conflict of interests
The authors declare that there are no competing interests.
Authors’ contributions
MG performed literature searches, study coding, analysis, and prepared the manuscript; AM conceived and directed the study, performed study coding, and edited the manuscript; SSchneider performed literature searches and study coding, and edited the manuscript; SSohl performed literature searches and study coding, and edited the manuscript; SK performed literature searches and study coding. Authors read and approved the final manuscript for submission.
References
[1] Newport F. Religion is most important
to blacks, women, and older Americans: Self-reported importance of religion
decreases with education. In: Gallup News Service; 2006. Available at
http://www.gallup.com/poll/25585/Religion-Most-Important-Blacks-Women-Older-Americans.aspx
[Last Accessed November 20, 2011].
[2] Newport F. More than 9 in 10 Americans
continue to believe in god: Professed belief is lower among younger Americans,
easterners, and liberals. In: Gallup; 2011. Available at
http://www.gallup.com/poll/147887/Americans-Continue-Believe-God.aspx. [Last
Accessed November 20, 2011].
[3] Newport F. Christianity remains
dominant religion in the United States: Majority still says religion is very
important in their lives. In: Gallup; 2011. Available at
http://www.gallup.com/poll/151760/Christianity-Remains-Dominant-Religion-United-States.aspx
[Last Accessed April 12, 2012].
[4] Quackenbos S, Privette G, Klentz B.
Psychotherapy: Sacred or secular? Journal of Counseling & Development
1985;63:290
[5] Fouad N, Arredondo P, D’Andrea M, Ivey
A. Guidelines on multicultural education, training, research, practice, and
organizational change for psychologists- American Psychological Association. In:
Association AP ed: American Psychological Association; 2002:103.
[6] Fuertes JN, Stracuzzi TI, Bennett J,
et al. Therapist multicultural competency: A study of therapy dyads.
Psychotherapy: Theory, Research, Practice, Training 2006;43:480-490
[Pubmed]
[7] Wade NG, Worthington EL, Vogel DL.
Effectiveness of religiously tailored interventions in Christian therapy.
Psychotherapy Research 2007;17:91-105.
[8] Worthington EL, Jr., Kurusu TA,
McCollough ME, Sandage SJ. Empirical research on religion and psychotherapeutic
processes and outcomes: A 10-year review and research prospectus. Psychological
Bulletin 1996;119:448-487.
[9] Halstead MT, Fernsler JI. Coping
strategies of long-term cancer survivors. Cancer Nursing 1994;17:94-100 [Pubmed].
[10]. Agarwal M, Hamilton JB, Crandell
JL, Moore CE. Coping strategies of African American head and neck cancer
survivors. Journal of Psychosocial Oncology 2010;28:526-538 [Pubmed].
[11]. Hamilton JB, Stewart BJ, Crandell
JL, Lynn MR. Development of the Ways Of Helping Questionnaire: A measure of
preferred coping strategies for older African American cancer survivors.
Research in Nursing & Health 2009;32:243-259.
[12]. Sherman AC, Simonton S, Adams DC,
Vural E, Hanna E. Coping with head and neck cancer during different phases of
treatment. Head & Neck 2000;22:787-793 [Pubmed].
[13] Al-Azri M, Al-Awisi H, Al-Moundhri
M. Coping with a diagnosis of Breast Cancer: Literature review and implications
for developing countries. Breast Journal 2009;15:615-622 [Pubmed].
[14]. Gall TL, Guirguis-Younger M,
Charbonneau C, Florack P. The trajectory of religious coping across time in
response to the diagnosis of breast cancer. Psycho-Oncology 2009;18:1165-1178 [Pubmed].
[15] Thomas SF, Marks DF. The measurement
of coping in breast cancer patients. Psycho-Oncology 1995;4:231-237.
[16] Cole B, Pargament K. Re-creating
your life: A spiritual/psychotherapeutic intervention for people diagnosed with
cancer. Psycho-Oncology 1999;8:395-407 [Pubmed].
[17]. Doyle D. Have we looked beyond the
physical and psychosocial? Journal of Pain and Symptom Management 1992;7:302-311 [Pubmed].
[18]. Park CL, Folkman S. Meaning in the
context of stress and coping. Review of General Psychology 1997;1:115-144.
[19]. Baugh JR. Gaining control by giving
up control: Strategies for coping with powerlessness. In: Miller WR, Martin JE
eds, Behavior therapy and religion: Integrating spiritual and behavioral
approaches to change. Thousand Oaks, California: Sage Publications, Inc;
1988:125-138.
[20] Rayburn CA. Psychotherapy with
Seventh-Day Adventists. In: Richards PS, Bergin AE eds, Handbook of
psychotherapy and religious diversity. Washington, DC: American Psychological
Association; 2000:211-234.
[21] Langman PF. Including Jews in
multiculturalism. Journal of Multicultural Counseling & Development
1995;23:222-236.
[22] Weaver AJ, Kline AE, Samford JA, et
al. Is religion taboo in psychology? A systematic analysis of research on
religion in seven major American Psychological Association journals: 1991–1994.
Journal of Psychology and Christianity 1998;17:220-232.
[23]. Larson DB, Pattison EM, Blazer DG,
Omran AR, Kaplan BH. Systematic analysis of research on religious variables in
four major psychiatric journals, 1978-1982. The American Journal Of Psychiatry
1986;143:329-334 [Pubmed].
[24] Schlosser LZ, Ali SR, Ackerman SR,
Dewey JJH. Religion, ethnicity, culture, way of life: Jews, Muslims, and
multicultural counseling. Counseling and Values 2009;54:48-64.
[25] Weber S, Pargament K, Kunik M, Lomax
J, Stanley M. Psychological distress among religious nonbelievers: A systematic
review. Journal of Religion & Health 2012;51:72-86.
[26] Hwang K, Hammer JH, Cragun RT.
Extending religion-health research to secular minorities: Issues and concerns.
Journal of Religion and Health 2011;50:608-622 [Pubmed].
[27] Ano GG, Vasconcelles EB. Religious
coping and psychological adjustment to stress: A meta-analysis. Journal of
Clinical Psychology 2005;61:461-480 [Pubmed].
[28] Masters KS, Spielmans GI, Goodson
JT. Are there demonstrable effects of distant intercessory prayer? A
meta-analytic review. Annals Of Behavioral Medicine: A Publication Of The
Society Of Behavioral Medicine 2006;32:21-26 [Pubmed].
[29]. Masters KS, Spielmans GI. Prayer
and health: Review, meta-analysis, and research agenda. Journal of Behavioral
Medicine 2007;30:329-338 [Pubmed].
[30] Roberts L, Ahmed I, Hall S, Davison
A. Intercessory prayer for the alleviation of ill health. Cochrane Database of
Systematic Reviews 2009 [Pubmed].
[31] Hodge DR, Horvath VE. Spiritual
needs in health care settings: A qualitative meta-synthesis of clients'
perspectives. Social Work 2011;56:306-316 [Pubmed].
[32]. Bergin AE. Religiosity and mental
health: A critical reevaluation and meta-analysis. Professional Psychology:
Research and Practice 1983;14:170-184.
[33] Sawatzky R, Ratner PA, Chiu L. A
meta-analysis of the relationship between spirituality and quality of life.
Social Indicators Research 2005;72:153-188.
[34] Hall DE. Religious attendance: More
cost-effective than lipitor? Journal Of The American Board Of Family Medicine:
JABFM 2006;19:103-109 [Pubmed].
[35] Edwards A, Pang N, Shiu V, Chan C.
The understanding of spirituality and the potential role of spiritual care in
end-of-life and palliative care: A meta-study of qualitative research.
Palliative Medicine 2010;24:753-770 [Pubmed].
[36]. McCullough ME, Hoyt WT, Larson DB,
Koenig HG, Thoresen C. Religious involvement and mortality: A meta-analytic
review. Health Psychology 2000;19:211-222 [Pubmed].
[37] Richards PS, Bergin AE. Review of
"Handbook of Psychotherapy and Religious Diversity". Cultural Diversity and
Ethnic Minority Psychology 2001;7:399-400.
[38] Schreiber JA, Brockopp DY.
Twenty-five years later--what do we know about religion/spirituality and
psychological well-being among breast cancer survivors? A systematic review.
Journal Of Cancer Survivorship: Research And Practice 2012;6:82-94 [Pubmed].
[39] Moyer A, Sohl SJ, Knapp-Oliver SK,
Schneider S. Characteristics and methodological quality of 25 years of research
investigating psychosocial interventions for cancer patients. Cancer Treatment
Reviews 2009;35:475-484 [Pubmed].
[40] Moyer A, Goldenberg M, Hall MA, Knapp-Oliver SK, Sohl SJ, Sarma EA, Schneider S. Mediators of change in psychosocial interventions for cancer patients: A systematic review. Behavioral Medicine,
2012; 38, 90-104 [Pubmed].
[41] Milot AS, Ludden AB. The effects of
religion and gender on well-being, substance use, and academic engagement among
rural adolescents. Youth & Society 2009;40:403-425.
[42] Sun F, Roff LL, Klemmack D, Burgio
LD. The influences of gender and religiousness on Alzheimer disease caregivers'
use of informal support and formal services. Journal of Aging & Health
2008;20:937-953 [Pubmed].
[43] Wachholtz A, Sambamoorthi U.
National trends in prayer use as a coping mechanism for health concerns: Changes
from 2002 to 2007. Psychology of Religion and Spirituality 2011;3:67-77.
[44]. Maselko J, Kubzansky LD. Gender
differences in religious practices, spiritual experiences and health: Results
from the US General Social Survey. Social Science & Medicine 2006;62:2848-2860 [Pubmed].
[45]. McFarland MJ. Religion and mental
health among older adults: Do the effects of religious involvement vary by
gender? Journals of Gerontology Series B: Psychological Sciences & Social
Sciences 2010;65B:621-630 [Pubmed].
[46]. Wink P, Dillon M, Prettyman A.
Religion as moderator of the sense of control--health connection: Gender
differences. Journal of Religion, Spirituality & Aging 2007;19:21-41.
[47] Jacobs-Lawson JM, Schumacher MM,
Hughes T, Arnold S. Gender differences in psychosocial responses to lung cancer.
Gender Medicine 2010;7:137-148 [Pubmed].
[48]. Taylor RJ, Chatters LM. Importance
of religion and spirituality in the lives of African Americans, Caribbean Blacks
and Non-Hispanic Whites. Journal of Negro Education 2010;79:280-294.
[49]. Chatters LM, Taylor RJ, Bullard KM,
Jackson JS. Race and ethnic differences in religious involvement: African
Americans, Caribbean Blacks and non-Hispanic Whites. Ethnic and Racial Studies
2009;32:1143-1163 [Pubmed].
[50] Randolph-Seng B, Nielsen ME, Bottoms
BL, Filipas H. The relationship between ethnicity, Christian orthodoxy, and
mental health. Mental Health, Religion & Culture 2008;11:795-805.
[51] Blaine B, Crocker J. Religiousness,
race, and psychological well-being: Exploring social psychological mediators.
Personality and Social Psychology Bulletin 1995;21:1031-1041.
[52]. Zinnbauer BJ, Pargament KI, Cole B, Rye MS, Butfer EM, Belavich TG, Hipp KM, Scott AB, Kadar JL. Religion and spirituality: Unfuzzying the fuzzy. Journal for the Scientific Study of Religion
1997; 36:549-564.
[53]. Samarel N, Tulman L, Fawcett J.
Effects of two types of social support and education on adaptation to
early-stage breast cancer. Research in Nursing & Health 2002;25:459-470 [Pubmed].
[54] Puig A. The efficacy of art therapy
to enhance emotional expression, spirituality, and psychological well-being of
newly diagnosed Stage I and Stage II breast cancer patients. In. Gainesville,
Florida: University of Florida; 2004.
[55] Peterman AH, Fitchett G, Brady MJ,
Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The
Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale
(FACIT-Sp). Annals of Behavioral Medicine 2002;24:49-58 [Pubmed].
[56] Pargament KI, Koenig HG. The many
methods of religious coping: Development and initial validation of the RCOPE.
Journal of Clinical Psychology 2000;56:519-543 [Pubmed].
[57]. Klauer T, Filipp S. Trierer Skalen
zur Krankheitsbewaeltigung. Göttingen: Hofgrefe. Göttingen: Hofgrefe.; 1993.
[58]. Garland SN, Carlson LE, Cook S,
Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress
reduction and healing arts programs for facilitating post-traumatic growth and
spirituality in cancer outpatients. Support Care Cancer 2007;15:949-961 [Pubmed].
[59] Moadel AB, Shah C, Wylie-Rosett J,
et al. Randomized controlled trial of yoga among a multiethnic sample of breast
cancer patients: Effects on quality of life. Journal of Clinical Oncology
2007;25:4387-4395 [Pubmed].
[60] Nidich SI, Fields JZ, Rainforth MV,
et al. A randomized controlled trial of the effects of transcendental meditation
on quality of life in older breast cancer patients. Integrated Cancer Therapy
2009;8:228-234.
[61] Ferrell BR, Grant M. Quality of life
instrument - breast cancer patient version. In: National Medical Center and
Beckman Research Institute; n.d.
[62]. Warner AS. Exploration of
psychological and spiritual well-being of women with breast cancer participating
in the Art of Living program. In. Palo Alto California: Institute of
Transpersonal Psychology; 2006.
[63]. Ando M, Morita T, Okamoto T,
Ninosaka Y. One-week Short-Term Life Review interview can improve spiritual
well-being of terminally ill cancer patients. Psychooncology 2008;17:885-890 [Pubmed].
[64] Breitbart W, Rosenfeld B, Gibson C,
et al. Meaning-centered group psychotherapy for patients with advanced cancer: a
pilot randomized controlled trial. Psychooncology 2010;19:21-28.
[65]. Gard T, Brach N, Hölzel BK, et al.
Effects of a yoga-based intervention for young adults on quality of life and
perceived stress: The potential mediating roles of mindfulness and
self-compassion. . The Journal of Positive Psychology 2012;7:165-175.
[66] Gonen G, Kaymak SU, Cankurtaran E,
et al. The factors contributing to death anxiety in cancer patients. Journal of
Psychosocial Oncology, 30, 347-358. Journal of Psychosocial Oncology
2012;30:347-358.
[67] Exline JJ, Park CL, Smyth JM, Carey
MP. Anger toward God: Social-cognitive predictors, prevalence, and links with
adjustment to bereavement and cancer. . Journal of Personality and Social
Psychology 2011;100:129-148 [Pubmed].
[68] Ellison C, Bradshaw M, Kuyel N,
Marcum J. Attachment to God, stressful life events, and changes in psychological
distress. . Review of Religious Research 2012;53:493-511.
[69] Smith-Stoner M. End-of-life
preferences for atheists. Journal of Palliative Medicine 2007;10:923-928 [Pubmed].
[70]. Research AAfC (n.d.) Federal cancer research funding. http://www.aacr.org/home/public--media/science-policy--government-affairs/resources-for-policymakers/federal-cancer-research-funding.aspx#4. Accessed May 21 2012
[71] Institute NC (2011) Cancer research funding. National Cancer Institute. http://www.cancer.gov/cancertopics/factsheet/NCI/research-funding. Accessed May 21 2012
[72] McLean CP, Anderson ER. Brave men
and timid women? A review of the gender differences in fear and anxiety.
Clinical Psychology Review 2009;29:496-505.
[73] Pierce KA, Kirkpatrick DR. Do men
lie on fear surveys? Behaviour Research And Therapy 1992;30:415-418 [Pubmed].
[74]Vasegh S. Cognitive therapy of
religious depressed patients: Common concepts between Christianity and Islam.
Journal of Cognitive Psychotherapy 2011;25:177-187.

