Research

Urinary tract infection – evaluation of β-glucan, mannose and cranberry extract
* Vetvicka V *Vetvickova J
- * University of Louisville, Department of Pathology, Louisville, KY, USA
- Submitted: Wednesday, December 16 2020;
- Accepted: Tuesday, December 29, 2020 ,
- Published: Tuesday, December 29, 2020 ,
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Urinary tract infection represents common problem for both general public and for athletes. Repeated infections are, at least partly, caused by depressed immune system; β-glucan is well-established immunomodulator with known helping effects in all types of infections. Therefore, we decided to compare various natural molecules in order to experimentally confirm the hypothesis that β-glucan alone or in combination with some additional natural molecule can have beneficial effects in this type of infection.
Patients and methods
The aim of this study was to evaluate the effects of some natural molecules as potential food supplement in UTI. For these experiments we used β-glucan, mannose, cranberry extract and their combinations.
Results
The highest effects on lowering the bacterial load in kidney and bladder had combination of β-glucan-cranberry extract followed by β-glucan alone. Based on our findings.
Conclusion
We can conclude that the highest effects have a β-glucan-cranberry extract combination.
Keywords
Urinary tract infection, β-Glucan, Cranberry, Mannose, Infection
Introduction
Urinary tract infection (UTI) is a common disease usually with mild conditions but in vulnerable patients such as immunocompromised individuals might require hospitalization. The primary agents are strains of pathogenic Escherichia coli, which usually migrate from the intestine through the urethra to the bladder and kidney. UTIs are among the most common bacterial infections with more than 150 million patients each year. UTI is generally defined as the presence of bacteria (over 100,000 cells/ml) in the urine. Treatments of choice are antimicrobials such as fosfomycin and nitrofurantoin, but alarming increase in microbial resistance is a global threat to common medical treatments leading to raising interest in non-antibiotic treatments.
Non-pharmacological oral supplements including cranberry [1], probiotics [2] or xyloglucan [3] have been used. In case of xyloglucan, the mechanism of action is supposed to be improvement of neutrophil infiltration and formation of protective barrier [4]. Similar effects were found for hibiscus and propolis [5], leading to a medical device containing a combination of all three components [6]. Another commonly used natural substance is cranberry juice or extracts rich in anthocyanins. It is used either alone or in combination with mannose [7]..
In our study we focused our attention on comparison of the effects of cranberry, mannose and β-glucan. The effects of β-glucan on anti-infection immunity are among the oldest effects of glucan studied. It has been demonstrated that glucans protect against infection in numerous experimental models and was shown to enhance antibiotic efficacy in infections with antibiotic-resistant bacteria. The protective effect of glucans was evidenced in experimental infection with Leishmania major and Leishmania donovani, Candida albicans, Toxoplasma gondii, Streptococcus suis, Plasmodium berghei, Staphylococcus aureus, Escherichia coli, Mesocestoidescorti, Trypanosoma cruzi and Eimeria vermiformis[8]. Our preliminary results using mouse model of UTI suggested promising results [9].
Evidence from animal studies demonstrates that glucan can reduce the amount of conventional antibiotics required in infectious conditions such as peritonitis (inflammation of the membrane lining of the abdominal and pelvic cavities). In mice infected with bacteria to induce peritonitis, a combination of b-glucan and standard antibiotics increased the long-term survival by 56%. Bacterial counts were noticeably down within eight hours of the injection and the numbers of key immune cells were markedly higher. Bowders et al.,[10]studied the stimulation of human macrophages in trauma patients and found that β-glucan therapy strongly decreased septic morbidity. A multicenter, double blind study found the optimal dosage of β-glucan in high-risk surgical patients. In addition, these studies demonstrated the safety and efficacy of β-glucan in surgical patients who underwent major thoracic or abdominal surgery. Since no adverse drug experiences associated with b-glucan infusion have been found, β-glucan-treated patients had significantly lower levels of infections. The biological effects of β-glucan on anti-infectious immunity are two-fold: macrophages are activated to produce various substances, directly killing the bacteria and stimulation of B lymphocytes to produce more antibodies.
The aim of our study was to directly compare the effects of three natural products, β-glucan, D-mannose and cranberry extract and their combination on E.coli-based urinary tract infection.
Material and Methods
Animal
Female, 8 week old BALB/c mice were purchased from the Jackson Laboratory (Bar Harbor, ME). All animal work was done according to the University of Louisville IACUC protocol. Animals were sacrificed by cervical dislocation. Nine mice/group (504 mice total) were used.
Material
β-Glucan was purchased from Biorigin (Sao Paulo, Brazil) and it is a yeast-derived, insoluble b-glucan of 75% purity. D-mannose was purchased from DSL Food (Litovel, Czech Republic), 90% cranberry juice powder from (Evear Extractions, Coutures, and France). Same amount of each material (100 bg/mouse/day) was used in supplementation for 7, 10, 14 or 21 days.
Urinary tract infection
Urinary tract infection was induced via direct inoculation of 10 bl of E. coli into the bladder using a syringe equipped with soft polyethylene tubing as previously described [11, 12].Briefly, the bladder was emptied by gentle pressure. The appropriate bacterial suspension was then instilled into the bladder while animals were kept under ether anesthesia. For urethral inoculation, a syringe fitted with 0.61-mm outside-diameter polyethylene tubing (Intramedic PE-I 0; Becton Dickinson, Parsippany, NJ) was used. Tested samples were used orally (forced feeding) at 4 mg/kg doses for 14 days. Mice were sacrificed at various intervals (6 h, 24 h, and 72 h) after infection and bladder and right kidney were aseptically collected from each animal. After weighing, organs were homogenized in sterile PBS. Obtained material was centrifuged to discard the tissue fragments. Appropriate dilutions were plated on Petri dishes with Levine EMB agar (Fisher Scientific (Waltham, MA, USA) and incubated at 37oC. Colony-forming units (CFU/mg of tissue) were evaluated 24 h later.
Statistics
Student’s t-test was used to statistically analyze the data. Data at p<0.05 were considered significantly different..
Results
Using a model of mouse urinary tract infection, we observed the appearance of E. coli as CFU in bladder and kidney after 7 and 10 days of oral treatment. In the first part of our study, we measured the level of bacteria in the bladder at various intervals after the infection. Data summarized in (Figure1) show significant effects of β-glucan on lowering the CFU. Cranberry alone also significantly lowered the bacterial load, mannose alone had no effects. When we evaluated the combination of or samples, the highest effects were found in β-glucan-cranberry combination. Similar situation was found when we supplemented the animals for a longer period (14 days instead of 7 days in Figure1). The lowering of bacterial load was stronger and even the mannose-cranberry combination showed significant effects (Figure2).
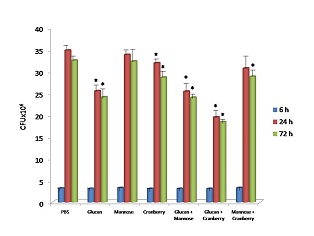
Figure 1 Effects of tested samples on lowering the CFU in kidney after 7 days of supplementation. Results represent mean from three experiments ± SD.*Represents significant differences between the PBS and treated mice at P≤ 0.05 level.

Figure 2 Effects of tested samples on lowering the CFU in kidney after 14 days of supplementation. Results represent mean from three experiments ± SD.*Represents significant differences between the PBS and treated mice at P≤ 0.05 level.
Next we focused on kidney. Level of bacteria after 10 days supplementation was measured at day 1, day 3 and day 7 post infections. The results shown in (Figure3) demonstrate the steadily increasing number of CFUs in control animals. Cranberry extract and β-glucan again significantly lowered the bacterial load, mannose alone showed no activity. All combinations were active; the mannose-cranberry combination was the least effective. When we repeated the same experimental design 21 days after start of the supplementation, all tested material and their combinations were similarly effective, with exception of mannose alone ( (Figure4).

Figure 3 Effects of 10 days of supplementation on levels of bacteria in bladder. Levels of bacteria were measured at day 1, day 3 and day 7 post infections. Results represent mean from three experiments ± SD.*Represents significant differences between the PBS and treated mice at P≤ 0.05 level.

Figure 4 Effects of 21 days of supplementation on levels of bacteria in bladder. Levels of bacteria were measured at day 1, day 3 and day 7 post infections. Results represent mean from three experiments ± SD.*Represents significant differences between the PBS and treated mice at P≤ 0.05 level.
Discussion
Conventional therapy of UTI often results in high reoccurrence rate, increase risk of candida infection and possible antibiotic resistance. All together, the search is still on for possible simple, inexpensive and reliable treatment, including nutritional supplements and natural immunomodulators.
Cranberry (Vaccinium macrocarpon) extracts contain high levels anthocyanidins and D-mannose and are traditionally used for the treatment and prevention of UTI starting with Native American medicine. Current literature confirmed that cranberry juice inhibit the adherence of E. coli to the wall of urinary tract and ameliorate the problems connected with UTI [13, 14]. Long term supplementation with cranberry juice resulted in significant decrease of relapses of UTI [15]. On the other hand, the situation is not clear, as numerous studies found little or even no protection against UTI. A double-blind, placebo-controlled clinical trial evaluating 319 women found to effects of cranberry juice in prevention of recurrent urinary tract infections [16].
D-Mannose is known to bind to the type 1 pili of various enteric bacteria resulting in a blockage of their adhesion to the uroepithelial cells. Prophylactic D-mannose supplementation was found to decrease the risk of recurrent URI [17].
β-Glucans were originally considered to be nonspecific stimulators of cellular immunity. Later, b-glucans have also been established as anti-infectious agents improving the health in every type of infection tested, including respiratory tract infection [9, 18-19].
Our study focused on direct comparison of these three substances and their combinations. From our results we can reach several conclusions – both β-glucan and cranberry extract strongly ameliorated the effects of E. coli infection by decreasing the bacterial load in bladder and kidney. Whereas β-glucan most probably acts via stimulation of various branches of immune reactions, mechanisms of the effects of cranberry are still unclear and the hypothesis about proanthocyanidins found in cranberry extracts interfering with the bacteria’s ability to adhere to the cells in the bladder wall are not fully established. Surprisingly, D-mannose alone showed no significant effects. When we tested the various combinations, β-glucan-cranberry combination showed the strongest effects, whereas mannose-cranberry combination in some cases blocked the palliative effects of cranberry extract.
We have to remember that, as in case of many natural materials, the amount of active ingredient that each product contains is not necessarily consistent. Therefore, some products may not have enough of the active ingredient to be effective in preventing bacteria from sticking to the bladder wall. This, however, does not include β-glucan, as it is offered as a more or less purified molecule and not as an extract.
Conclusion
From our study we can conclude that the use of β-glucan in UTI has a strong potential to offer improvements of conditions via suppressing of bacterial load in affected organs. Highly concentrated cranberry extract showed solid effects too, but for commercial purposes, it might be difficult to be sure about the quality of available extracts.
Conflict of interest
The authors confirm that this article's content has no conflict of interest.
Statement of Ethics
The study was approved by the Institute Animal ethics committee. The copy of the approval letter is available with the authors.
Availability of Data
The data is available from authors on reasonable request.
Authors contribution
VV: Designed the study and prepared the manuscript
VJ: conducted the study and edited the study Both authors approved the final version of the article for publication and take the responsibility for the article.
Funding:
Nil
Acknowledgement
Nil
References
[1]Gupta A, Dwivedi M, Mahdi AA, Nagana Gowda GA, Khetrapal CL, Bhandari M.(2012). Inhibition of adherence of multi-drug resistant E. coli by proanthocyanidin. Urol Res. 40:143-50 [PubMed]
[2]Chisholm AH. (2015). Probiotics in preventing recurrent urinary tract infections in women: A literature review. Urol Nurs. 35:18-21[PubMed]
[3]De Servi B, Ranzini F, Pique N. (2016). Effect of Utipro (containing gelatin-xyloglucan) against Escherichia coliinvasion of intestinal epithelial cells: Results of an in vitro study. Future Microbiol. 11:651-658.
[4]Esposito E, Campolo M, Casili G, Lanza M, Franco D, Fillipone A, et al. Protective effects of xyloglucan in association with the polysaccharide gelose in an experimental model of gastroenteritis and urinary tract infections. Int J Mol Sci. 2018; 19, doiL10.3390/ijms19071844. [PubMed] [PMC Full Text]
[5]Fraile B, Alcover J, Royuela M, Rodriguez D, Chaves C, Palacios R, et al. Xyloglucan, hibiscus and propolis for the prevention of urinary tract infections: results of in vitro studies. Future Microbiol. 2017;12:721-31. [PubMed]
[6]Costache RC, Novac B, Bardan T.R., Agapie DN, Edu A. Xyloglucan + gelose combination versus placebo as adjuvant therapy to first-line antimicrobial for uncomplicated urinary tract infection in adults. Urol Int. 2019; 102:468-75.[PubMed]
[7]Minatelli JA, Hill WS. Method of preventing, controlling and ameliorating urinary tract infections using a synergistic cranberry derivative and D-mannose composition U.S. Patent Application D.N.20090226548 A1, 2009.
[8]Vetvicka V, Novak M. Biological action of β-glucan. In V. Vetvicka, M. Novak (Eds.), Biology and Chemistry of Beta Glucan, 2011; Vol. 1, pp. 10-18, Bentham Science.
[9]Vetvicka V, Vetvickova J. Anti-infectious and anti-tumor activities of b-glucan. Anticancer Res. 2020; 40:3139-45.[PubMed]
[10]Bowders GJ, Patchen ML, MacVittie TJ, Hirsch EF, Fink MP. Glucan enhances survival in an intraabdominal infection model. J Surg Res.1989; 47: 183-8. [PubMed]
[11]Hopkins WJ, Hall JA, Conwaz BP, Uehling DT. Induction of urinary tract infection by intraurethral inoculation with Escherichia coli: Refining the murine model. J Inf Dis. 1995; 171:462-5. [PubMed]
[12]Rosen DA, Hung CS, Kline KA, Hultgren SJ. Streptozocin-induced diabetic mouse model of urinary tract infection. Infect Immun. 2008; 76:4290-8. [PubMed] [PubMed]
[13]Beerepoot MA, ter Riet G, Nys S, van der Wal WM, de Borgie CA, de Reijke TM, et al. Cranberries vs. antibiotics to prevent urinary tract infections: a randomized double-blind noninferiority trial in premenopausal women. Arch Intern Med. 2011; 171:1270-8.[PubMed]
[14]Oppel M. Cranberry effective in treating UTIs during pregnancy and lactation Herbalgam 2008; 80:31.
[15]Takahashi S, Hamasuna R, Yasuda M, Arakawa S, Tanaka S, Ishikawa S, et al. A randomized clinical trial to evaluate the preventive effect of cranberry juice (UR65) for patients with recurrent urinary tract infection. J Inf Chemotherap. 2013; 19:112-7. [PubMed]
[16]Barbosa-Cesnik C, Brown MB, Buxton M, Zhang L, DeBusscher J, Foxman B. Cranberry juice fails to prevent recurrent urinary tract infection: Results from a randomized placebo-controlled trial. Clin Infect Dis., 2011; 52:23-30[PubMed][PMC Full Text]
[17]Kranjcec B, Papes D, Altarac S. D-Mannose powder for prophylaxis of recurrent urinary tract infections in women: a randomized clinical trial. World J Urol. 2014; 32:79-84.[PubMed]
[18]Dharsono T, Rudnicka K, Wilhelm M and Schoen C. Effects of yeast (1,3)-(1,6)-beta-glucan on severity of upper respiratory tract infections: A double-blind, randomized, placebo-controlled study in healthy subjects. J Am Coll Nutr. 2019;38(1): 40-50. PMID: 30198828. DOI: 10.1080/07315724.2018.1478339[PubMed]
[19]Mah E, Kaden VN, Kelley KM and Liska DJ. Soluble and insoluble yeast beta-glucan differentially affect upper respiratory tract infection in marathon runners: A double-blind, randomized placebo-controlled trial. J Med Food 2019; 23(4): 416-9. PMID: 31573387. DOI: 10.1089/jmf.2019.0076[PubMed]

