Original Article

Direct Immunofluorescence in Lichen Planus and Lichen Planus like Lesions
* Reema Bhushan, *Shilpi Agarwal, $Ram Chander, * Kiran Agarwal,
- *Department of Pathology, Lady Hardinge Medical College, New Delhi, India
- $ Department of Dermatology, Lady Hardinge Medical College, New Delhi, India
- Submitted: Sunday, January 15, 2017:
- Accepted: Tuesday, January 31, 2017
- Published:: Thursday, February 2, 2017
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
The direct immunofluorescence examination (DIF) in lichen planus (LP) and lichen planus like lesions can show deposition of multiple immunoreactants at dermoepidermal junction (DEJ) and cytoid bodies (CB).
Patients and Methods
Fifty one cases of lichen planus and lichen planus like lesions were included in the study on the basis of clinical and histological criteria at Department of Pathology, Lady Hardinge Medical College from November 2012 to March 2014. The results of direct immunofluorescence was analysed in these cases.
Results
Among lichen planus (LP), DIF positivity at dermoepidermal junction (DEJ) was seen in 25/33 (75.6%) cases followed by deposit at cytoid bodies in 18/33 (54.5%) cases. The immunoreactivity at DEJ was most commonly seen with fibrinogen in 24/33 (72.7%) cases. DIF positivity at cytoid bodies was most commonly seen with C3 in 12/33 (36.3%) cases. Among lichen planus pigmentosus (LPP), DIF positivity was seen in 9/13 (69.2%) cases. The deposit at DEJ was noted in 2/13 (15.3%) cases while deposit at cytoid bodies was seen in 8/13 (61.5%) cases. Most common immunoreactant at cytoid bodies was C3 in 5/13 (38.4%) cases. The sensitivity of histopathology and direct immunofluorescence for the diagnosis of lichen planus including lichen planus-like lesions was found to be 100% & 74.5% (LP-87.9% and LPP-69.2%) respectively.
Conclusions
The study showed that DIF is helpful in diagnosis of LP and LP like lesions. In LP, the shaggy fibrinogen deposit alone at DEJ & C3 alone or in combination of other immunoreactants at CB was found to be most characteristic
Key words
Direct immunofluorescence, Lichen planus, skinskin, pathology,
Introduction
Lichen planus (LP) is an idiopathic subacute or chronic inflammatory disease of the skin, mucous membranes and nails [1]. Cutaneous lichen planus is characterized by polygonal flat-topped, violaceous papules and plaques, which in some cases can be intensely itchy. The lesions may result in longstanding residual hyperpigmentation, especially in dark skinned patients [2]. According to one study LP represents 0.38% of all dermatology outpatients in India [3]. LP frequently occurs between the ages of 30 and 60 years without sexual or racial predilection [4].
The diagnosis of LP is based on the clinical character of the lesions and histological examination [5]. However, direct immunofluorescence (DIF) studies may be helpful in disease differentiation for cases with ambiguous features of other diseases, e.g. lupus erythematous (LE) [6]. This study was undertaken to analyze the role of direct immunofluorescence in the diagnosis of lichen planus and lichen planus like lesions.
Material and Methods
Fifty one cases of lichen planus and lichen planus like lesions were included in the study on the basis of clinical and histological criteria at Department of Pathology, Lady Hardinge Medical College from November 2012 to March 2014. A single 4mm punch biopsy of skin lesions was taken and it was bisected with one half sent for histopathological examination in 10% neutral formalin and other half in Michel’s medium (pH = 7.25) for direct immunofluorescence examination. Five µm thick tissue sections were cut for immunofluorescence study by a standardized method.
Slides of each case was stained with fluorescein isothiocyanate (FITC) conjugated antibodies directed against IgG, IgM, IgA, C3 and fibrinogen and incubated in dark at 37°c for 1 hour. After several washings in phosphate buffer saline (PBS), the slides were mounted in glycerine PBS mixture and viewed under the immunofluorescence microscope fitted with an UV light source, under ideal excitation and barrier filter combination. Each slide was assessed for presence or absence of immunoreactants, type of immunoreactant, site of deposition (basement membrane zone, cytoid body), pattern (linear, granular, homogenous, shaggy etc.) and intensity of fluorescence. The approval of Ethics Committee of Lady Hardinge Medical College was obtained prior to the study. Informed consent from the participants was also obtained.
Results
Fifty one cases comprised of lichen planus (LP, 33/51), lichen planus pigmentosus (LPP, 13/51), lichen planus hypertrophicus (LPH, 2/51), lichen planopilaris (LPPil, 1/51), lichen nitidus (L nitidus, 1/51) and lichen striatus (L striatus, 1/51) (Table 1).
| Diagnosis (n) |
HPE |
DIF |
Site |
| LP(33) |
100% |
87.9% |
DEJ(75.6%) followed by deposit at CB(54.5%) |
| LPP(13) |
100% |
69.2% |
CB(61.5%) followed by deposit at DEJ(15.4%) |
| LPH(2) |
100% |
NEG |
- |
| L Planopilaris (1) |
100% |
NEG |
- |
| L Nitidus (1) |
100% |
NEG |
- |
| L Striatus (1) |
100% |
NEG |
- |
The age distribution ranged from 5-69 years with slight female preponderance (50.99%). The cases of LP ranged from 5-68 years, cases of LPP ranged from 9-69 years. The mean age of LPH was 11.5 yrs. There was one case each of PPil, L nitidus and L striatus aged 30 years, 26 years and 12 years respectively.
The sensitivity of histopathology and direct immunofluorescence for the diagnosis of lichen planus including lichen planus-like lesions was found to be 100% & 74.5% (LP-87.9%; p value=0.114 and LPP-69.2%; p value=0.096) respectively. Among LP, DIF positivity with the deposit at DEJ was the commonest (25/33, 75.6%) followed by deposit at cytoid bodies (18/33, 54.5%). The immunoreactivity at DEJ was most commonly seen with fibrinogen alone (24/33, 72.7%) (Table 2).
| Immunoreactant |
DEJ |
CB |
| FIB |
24 |
0 |
| C3 |
0 |
4 |
| IgM |
0 |
3 |
| IgM+C3 |
1 |
3 |
| C3+IgG |
0 |
2 |
| IgG,C3,IgM |
0 |
1 |
| IgG |
0 |
1 |
| C3,IgM,IgA,IgG |
0 |
1 |
| FIB,IgG,IgA |
0 |
1 |
| IgA,IgM,C3 |
0 |
1 |
| IgA |
0 |
1 |
| Negative |
8 |
15 |
Among LPP, DIF positivity at cytoid bodies was seen in 8/13 (61.5%) cases, most commonly seen with C3 in 12/33 (36.3%) cases followed by IgM 9/33 (27.2%). The deposit at DEJ was noted in 2/13 (15.3%) cases, seen with fibrinogen (Table 3).
| Immunoreactant |
DEJ |
CB |
| C3 |
0 |
3 |
| FIB |
2 |
0 |
| FIB,IgM,C3 |
0 |
1 |
| IgM |
0 |
1 |
| IgM,C3 |
0 |
1 |
| IgA |
0 |
1 |
| IgG, IgM, |
0 |
1 |
| NEGATIVE |
11 |
5 |
Discussion
The cases of LP ranged from 5-68 years (mean age 32.42 yrs) in this study. Kulthanan et al., [4] and Dhar et al., [7] reported age range of 6-76 yrs and 29-45 years respectively among the LP patients. Cases of LPP ranged from 9-69 years (mean age 36.15 years) while Kanwar
et al., [8] reported age range between 13-62 years in his study on LPP. The mean age of LPH was 11.5 yrs. There was one case each of Lichen planopilaris, L nitidus and L striatus aged 30 years, 26 years and 12 years respectively. Chieregato C
et al., [9], Park et al., [10] and Mu
et al., [11] reported mean age of patients of Lichen planopilaris, Lichen nitidus and Lichen striatus as 52 years, 45 yrs and 4.6 years respectively.
Among LP, there was slight male predominance (51.5%) with M:F
ratio of 1.06:1 in concordance with Singh et al., [12] (M: F ratio =
3:2). Kulthanan et al., [4] reported an equal incidence in males & females
while Dhar et al., [7] reported M: F ratio of 1:6.5. Among LPP, there
was female predominance (61.5%) with M: F ratio being 1:1.6, similar to the
study of Kanwar et al., [8] (M:F= 1:1.2). Among LPH, both cases were
male. L PPil and L striatus have one female patient each while one case of L
nititdus was a male.
Direct Immunofluorescence Findings
Direct immunofluorescence positivity was seen in 29/33 (87.9%) cases of LP. Kulthanan
et al., [4] (Table 4)
| LP |
Kulthanan et al.(2007) |
This study |
| Mean age |
44.7 yrs |
32.4yrs |
| M:F ratio |
1:1 |
1.06:1 |
| HPE positivity |
100% |
100% |
| DIF positivity |
75% |
87% |
| DIF positivity at DEJ |
53% |
75% |
| MC immunoreactant at DEJ (out of total DIF positive cases) |
Fib (100%) |
Fib(96%) |
| DIF positivity at CB |
60% |
54.5% |
| MC immunoreactant at CB |
CB IgM(93%)> C3(47%) |
C3(36.3%)> IgM(27.2%) |
| Histo-immunological correlation |
75% |
87.9% |
and Kabir et al., [13] reported DIF positivity in 75% and 70.5% of LP respectively. Nine out of thirteen (69.3%) cases of LPP showed DIF positivity. Kanwar
et al., [8] reported DIF positivity in 14.2% cases of LPP (Table 5).
| LPP |
Kanwar et al |
This study |
| AGE |
13-62 yrs |
9-69 yrs |
| M:F |
1:1.2 |
1:1.6 |
| DIF+ |
14.2% |
69.3% |
| @CB |
- |
61.5% mc with C3(5/13) |
| @DEJ |
7.1% |
15.3% |
Among LP, DIF positivity with the deposit at DEJ (Figure 1).was the commonest seen in 25/33 (75.6%) followed by deposit at cytoid bodies in 18/33 (54.5%) cases. The immunoreactivity at DEJ was most commonly seen with fibrinogen alone in 24/33 (72.7%) cases. Kulthanan
et al., [4] found that either alone or in combination, the most common deposit at DEJ was fibrinogen (100%) followed by C3 (47%). Kabir
et al., [13] reported irregular deposits of fibrinogen/ IgM/ C3/ IgG at DEJ in 70.5% LP cases.
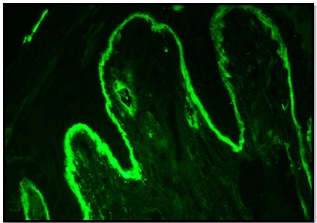
Figure 1: DIF of Lichen Planus showing shaggy deposits of fibrinogen at DEJ.
Among LPP, DIF positivity was seen in 9/13 (69.2%) cases. The deposit at DEJ was noted in 2/13 (15.3%) cases, seen with fibrinogen. Kanwar
et al., [8] reported DIF positivity with IgM and C3 at DEJ in 1/14 (7.1%) cases each. Among LP, DIF positivity at cytoid bodies, either alone or in combination, was most commonly seen with C3 in 12/33(36.3%) cases followed by IgM 9/33 (27.2%). Kulthanan
et al., [4] reported the cytoid bodies staining most commonly with IgM (93%) followed by C3 (47%) (Table 4).
Among the 13 cases of LPP, deposit at cytoid bodies was seen in 8/13 (61.5%) cases. Most common immunoreactant at cytoid bodies was C3 (Figure 2).in 5/13 (38.4%) cases followed by IgM in 4/13 (30.7%) cases. However, Kanwar
et al., [8] did not find positivity of any immunoreactant at cytoid bodies in his study on LPP. Among LP, a combination of DEJ (shaggy deposit) with deposit at CB was the commonest seen in 14/29 (48.3%) cases followed by DEJ (shaggy) alone seen in 10/29 (34.5%) cases. Chularojanamontri
et al., [14] also found that the most common pattern in LP (62%) was immunoreactant deposition at DEJ and CB (62.1%) followed by CB alone (29.3%).
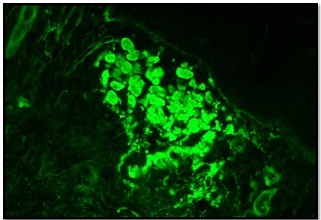
Figure 2: DIF of Lichen Planus showing C3 deposition at cytoid bodies in upper dermis.
In cases of LPP, the most common site of immunoreactions deposition was at CB alone, seen in 7/9 (77.8%) cases, while DEJ (shaggy) alone and a combination of DEJ (shaggy) and CB was seen in one case (11.1%) each. In our study, the immunoreactions deposition at DEJ and /or CB with fibrinogen, IgM, IgG & C3 was of strong intensity. Only IgA deposition at cytoid bodies was moderate in intensity. Nangia
et al., [15] observed that the intensity of DIF positivity was maximal in lesions of less than 3 months duration and which are associated with vasodilatation and dermal edema. The older lesions are DIF negative due to breakdown of fibrinogen by phagocytosis. Among LP, 29/33 (87.9 %) cases showed good histo-immunological correlation while among LPP, 9/13 (69.2%) cases showed good histo-immunological correlation. Kulthanan et al., [3] & Kabir
et al., [13] found histo-immunological correlation in 75% & 70.5% cases respectively among LP.
Histopathology was 100% sensitive for both LP and LPP while DIF was 87.9% (29/33) and 69.2% (9/13) sensitive respectively. Kulthanan
et al [4] also found that sensitivity of HPE for LP was higher (100%) as compared to DIF (75%). Although CBs can be found in whole lot of conditions, yet they are an important diagnostic finding in conditions like LP and DLE. Presence of CBs alone or in combination with other immunoreactions deposits at DEJ can help in differentiating the diseases presenting sometimes with close overlapping features [16]. Lichenoid eruptions represent a heterogeneous group of conditions that resemble idiopathic LP in terms of their clinical appearance and demonstrate a lichenoid tissue reaction. Direct immunofluorescence can be similar at times in these conditions. Thus, considering all three modalities
i.e. clinical features, histopathology and direct immunofluorescence, together can aid to reach a correct diagnosis [17].
Conclusion
The study showed that DIF is helpful in diagnosis of LP and LP like lesions. In LP, the shaggy fibrinogen deposit alone at DEJ & C3 alone or in combination of other immunoreactants at CB was found to be most characteristic while in LPP, deposit of C3 alone or in combination with other immunoreactants at CB is characteristic. However, DIF must always be used in conjunction with histopathology.
Authors' Contribution
Reema Bhushan: carried out the experiments
and interpreted the results, carried out the literature search and prepared the
draft manuscript, designed the study and performed the analysis, conceived the
study, participated in design and edited the final manuscript.
Shilpi Agarwal: interpreted the results, prepared the draft
manuscript, designed the study and performed the analysis, conceived the study,
participated in design and edited the final manuscript.
Ram Chander: conceived the study, participated in design and
edited the final manuscript
Kiran Agarwal: participated in design and edited the final
manuscript
All authors read and approved the final manuscript for
publication.
Conflict of Interests
The authors declare
that there are no conflicts of interests.
Ethical Considerations
The study was approved by Institute Ethics committee.
Funding
None Declared
Acknowledgement
None
References
[1].Boyd AS, Neldner KH. Lichen planus. J
Am Acad Dermatol 1991; 25(4):593–619.
[PubMed]
[2].Parihar A, Sharma S, Bhattacharya SN,
Singh UR. A clinicopathological study of cutaneous lichen planus. Journal of
Dermatology & Dermatologic Surgery 2015; 19:21–26. [Free
Fulltext]
[3].Bhattacharya M., Kaur I, Kumar B.
Lichen planus: a clinical and epidemiological study. J Dermatol
2000;27(9):576–582. [PubMed]
[4].Kulthanan K, Jiamton S, Varothai S,
Pinkaew S, Sutthipinittharm P. Direct immunofluorescence study in patients with
lichen planus. Int J Dermatol. 2007 Dec;46(12):1237-41. doi:
10.1111/j.1365-4632.2007.03396.x.
[PubMed]
[5].Daoud MS, Pittellkow MR. Lichen planus. In: Freedberg IM, Eisen AZ, Wolff K, eds. Fitzpatrick’s Dermatology in General Medicine, 6th ed. New York: McGraw-Hill, 2003: 463–477.
[6].Mutism DF, Adams BB. Immunofluorescence in dermatology. J Am Acad Dermatol 2001; 45: 803–822. PMID: 11712024.[PubMed]
[7].Dhar S, Kanwar AJ, Dawn G, Sehgal S. Paucity of immune complexes in skin lesions of lichen planus. Indian J Dermatol Venereol Leprol 1995; 61(1): 21-25. [PubMed]
[Free
Fulltext]
[8].Kanwar AJ, Dogra S, Handa S, Parsad D, Radotrat BD. A study of 124 Indian patients with lichen planus pigmentosus. Clinical and Experimental Dermatology 2003; 28: 481-485.
[PubMed]
[9].Chieregato C, Zini A, Barba A, Magnanini M, Rosina P. Lichen planopilaris: report of 30 cases and review of the literature. Int J Dermatol 2003 May; 42(5): 342-5.
[PubMed]
[10].Park SH, Kim SW, Noh TW, Hong KC,
Kang YS, Lee UH, Park HS, Jang SJ. A Case of Palmar Lichen Nitidus Presenting as
a Clinical Feature of Pompholyx. Ann Dermatol 2010; 22(2): 235–237. doi:
10.5021/ad.2010.22.2.235.
[PubMed] [PMC]
[11].Mu EW, Abuav R, Cohen BA. Facial
Lichen Striatus in Children: Retracing the Lines of Blaschko. Pediatric
Dermatology 2013; 30(3): 364-366. doi: 10.1111/j.1525-1470.2012.01844.
[PubMed]
[12].Singh OP, Kanwar AJ. Lichen panus in India: an appraisal of 441 cases. Int J Dermatol 1976; 15: 752-6.
[PubMed]
[13].Kabir AN, Das RK, Kamal M. Direct
Immunofluorescence Test of Skin Biopsy Samples – Results of 204 Cases. Dinajpur
Med Col J2009; 2(1): 8-12. [Free
Fulltext]
[14].Chularojanamontri L, Tuchinda P,
Triwongwaranat D, Pinkaew S, Kulthanan K. Diagnostic significance of colloid
body deposition in direct immunofluorescence. Ind J Dermatol Venereol Leprol
2010; 76: 373-377. doi: 10.4103/0378-6323.66583.
[PubMed]
[15].Nangia A, Kumar V, Logani KB. An immunopathological study of lichen planus. Ind J Dermatol Venereol Leprol 2000; 66(2):76-78.
[PubMed] [Free
Fulltext]
[16].Pranay T, Kumar AS, Chhabra S. Civatte Bodies: A Diagnostic Clue. Indian J Dermatol. 2013; 58(4): 327. doi: 10.4103/0019-5154.113974.
[PubMed] [PMC]
[17].Ismail SB, Kumar SKS, Zain RB. Oral lichen planus: etiopathogenesis, diagnosis, management and malignanat transformation. J Oral Sci 2007:49;89-106. [PubMed]
[Free
Fulltext]

