Case Report

Primary Ovarian Leiomyoma in Pregnant Woman: An Uncommon Tumor with an Unusual Presentation.
* Nihed Abdessayed *Meriem bel haj Salah *Raja Jouini, * Wafa Koubaa, *Ehsen ben Brahim, *Achraf Chadli Debbiche
- *Department of Pathology, Habib Thameur hospital, Tunis, Tunisia
- Submitted: Monday, December 5, 2016
- Accepted: Wednesday, January 11, 2017
- Published:: Sunday, January 15, 2017
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
Leiomyoma is a benign mesenchymal tumor that frequently occurs in uterus but rarely happens in ovary. Primary ovarian Leiomyoma is usually small, unilateral, and concomitantly seen with uterine leiomyoma in middle-aged and postmenopausal women. It is mostly diagnosed incidentally during pelvic examination.
Case presentation
We present the case of a 32-year old woman with a large anneal mass discovered at 18 weeks of pregnancy. Clinical course was marked by abdominal pain with fever. Histological examination of the ovarian mass reveled a spindle cell tumor without atypia or mitosis. Immunohistochemical staining with antibodies against smooth muscle actin confirmed the leiomyomatous nature of the tumor.
Conclusions
Ovarian Leiomyoma occurrence during pregnancy is more challenging for clinico-pathological diagnosis and operative management.
Keywords
ovary- Leiomyoma- pregnancy.
Introduction
Leiomyoma is one of the rarest solid tumors of ovary accounting for 0.5–1% of all benign ovarian tumors [1]. It is frequently unilateral and small, and it most commonly occurs in women aged 20-65 [2]. Patients are usually asymptomatic, and the tumor is often diagnosed incidentally [3, 4]. Its occurrence during pregnancy is uncommon. To our knowledge, only 5 cases have been reported in the literature, to date [3].
Case report
A 32-year-old woman, gravida1, at 18 weeks of intrauterine pregnancy, was admitted to gynecology department for abdomino-pelvic pain of 6 hours standing. Her past medical history was unremarkable. Emergency ultrasound examination revealed a single normal fetus in the uterus and a right adnexal hypo echoic solid mass of 6x5.5 cm in size with the characteristics of torsion. Due to the big size of the mass and to the presence of pain, the patient underwent a laparotomy with right salpingo-oophorectomy. During the following days, she complained of mild intermittent abdominal pain, associated with fever, vomiting, vaginal bleeding and uterine contractions. The uterus was movable with no tenderness, and was of the size corresponding to the gestational age. Nonetheless, ultrasound revealed a dead fetus. The resected ovary and fallopian tube were submitted for final examination. The ovarian mass measured 7x6.5cm at its greatest dimension, with a smooth and shiny surface. On sectioning, the tumor had a white-gray color and a whorled pattern at cut section. There was no normal recognizable ovarian tissue. The attached accompanying fallopian tube was unremarkable. Pathological examination demonstrated a well circumscribed but not encapsulated mass repulsing a residual ovarian parenchyma (Figure 1).
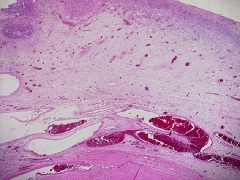
Figure 1: Bundles of smooth muscle cells lying under ovarian cortex (H&Ex100)
It consisted of typical smooth muscle cells forming strands and bundles arranged in a whorled interlacing pattern. Ischemic infarction focus was observed but without significant nuclear atypia or pleomorphism. Some hemorrhagic area and hyaline changes were also observed (Figure 2).
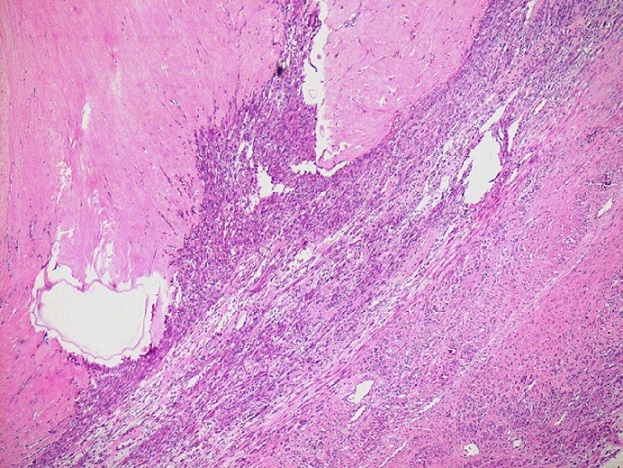
Figure 2: Spindle smooth muscle cells arranged in bundles with hyalinization area (H&Ex100)
Immunohistochemical staining with antibodies against smooth muscle actin (SMA) was performed and confirmed the leiomyomatous nature of the tumor (Figure 3).
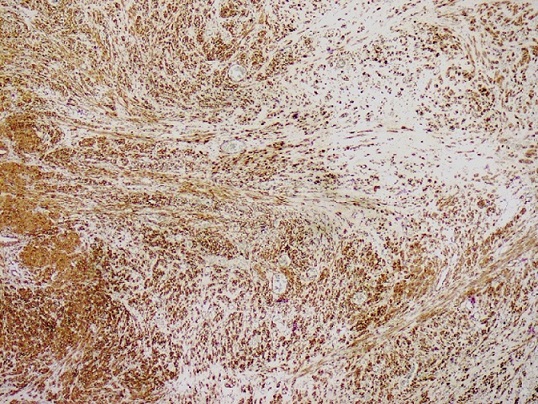
Figure 3: Immunohistochemical staining was positive for α-smooth muscle actin (Actin x200)
Discussion
Primary ovarian leiomyoma is a very rare benign tumor. Since its first description in 1862 by Sangalli et al, only 70 cases of this rare tumor have been reported [1, 2, 5]. Since the histogenesis of ovarian leiomyoma remains uncertain, several theories have been proposed regarding its potential origin. It is thought to originate from the walls of blood vessels in the ovarian hilus or from the smooth muscle fibers near the attachment of the ovarian ligament [3]. Other authors suggest the role of estrogens as stimulating factors since most tumors appear in nulliparous patients [6, 7]. Usually, primary ovarian leiomyoma presents as a unilateral mass, of 3cm in size of average. It is most often diagnosed by chance during routine physical examination or incidentally at surgery or autopsy. Occurrence during pregnancy, like our case is exceptional. To our knowledge five cases have been reported in pregnant women, till date. Huge tumors may be symptomatic; signs are not specific such as abdominal pain, a palpable mass, hydrothorax and/or ascites, hydronephrosis. Case reports show a unilateral predominance, with no predilection for left or right ovary. A few bilateral cases have been reported, most of them occurred in patients between the ages of 16 and 25 [8, 9]. Unilateral ovarian leiomyomas are frequently associated with other ipsilateral or contralateral ovarian lesions [1]. This association was found in 40% of the cases (mean age 45.8 years) reported by Doss et al., [6]. Furthermore, association with a concomitant uterine leiomyoma is more frequent suggesting a common pathogenesis of the two tumors [10, 11].
The gross characteristics of ovarian leiomyomas are variable. While some of them are solid, others have cystic components or are predominantly cystic. Hemorrhage, calcification and/or hyalinization are possible [5, 12]. Microscopically, diagnosis is easy. In fact, ovarian leiomyoma is identical to uterine counterpart. But, because of its rarity, several other tumors should be included in the differential diagnosis during histologic examination, especially leiomyosarcoma, angioleiomyoma, sclerosing stromal tumor and sex-cord tumors, such as fibroma/ thecoma [13]. Immunohistochemical study with smooth muscle specific staining (SMA and h-Caldesmon) is helpful to rule out differential diagnoses. It is also important to distinguish between primary ovarian leiomyomas and parasitic leiomyomas (pedunculated subserous leiomyomas), which become attached to the ovary after detaching from the uterus [3]. The common surgical approach of ovarian leiomyomas in middle-aged to elderly patients is by hysterectomy and bilateral salpingo-oophorectomy [2]. For symptomatic and large bulky masses, complete resection is recommended. For bilateral ovarian leiomyomas, bilateral oophorectomy is often required. In pregnant females, the laparoscopic approach for the management of benign ovarian tumors has become the preferred approach by surgeons, due to its efficacy and safety [1]. Regardless of treatment, primary ovarian leiomyoma is related to good prognosis. Reported cases in the literature highlight its benign course, which is similar to uterine leiomyoma.
Conclusion
Primary ovarian leiomyoma is a very rare tumor. Nevertheless, leiomyoma should be considered in the differential diagnosis when an ovarian tumor shows as a solid, spindle cell neoplasm. Appropriate muscle specific staining helps in correct diagnosis. However, its occurrence during pregnancy is more challenging for operative management.
Learning points:
-
This article highlights the rarity of this tumor
-
Discuss the clinical and pathological features of ovarian leiomyoma
-
The article emphasize on the challenging surgical management during pregnancy and its risks
Ethical Considerations
Written informed consent was obtained for publication of this case report.
Conflict of interest
The authors have no conflict of interest to declare.
Authors’ contributions
NA carried out the literature search and prepared the draft manuscript, MBS and NA interpreted the results, RJ, WK, EBB and ACD participated in design and edited the final manuscript. All authors read and approved the final manuscript for submission.
Acknowledgments
None
References
[1] Zhao X, Chen L, Zeng W, Jin B, DU W. Laparoscopic tumorectomy for a primary ovarian leiomyoma during pregnancy: A case report. Oncol Lett 2014;8:2523-6. [Pubmed]
[PMC fulltext]
[2] Van Esch EM, Van Wijngaarden SE, Schaafsma HE, Smeets MJ, Rhemrev JP. The diagnostic and therapeutic approach of a primary bilateral leiomyoma of the ovaries: a case report and a literature review. Arch Gynecol Obstet. 2011;283:1369-71.[Pubmed]
[3] Hsiao CH, Wang HC, Chang SL. Ovarian leiomyoma in a pregnant woman. Taiwan J Obstet Gynecol 2007 ;46:311-3 [Pubmed]
[Full
text]
[4] Matamala MF, Nogales FF, Aneiros J, Herraiz MA, Caracuel MD. Leiomyomas of the ovary. Int J GynecolPathol 1988;7:190-6 [Pubmed]
[5] Wei C, Lilic N, Shorter N, Garrow E. Primary ovarian leiomyoma: a rare cause of ovarian tumor in adolescence. J PediatrAdolesc Gynecol 2008;21:33-6.
[Pubmed]
[6] Doss BJ, Wanek SM, Jacques SM, Qureshi
F, Ramirez NC, Lawrence WD: Ovarian leiomyomas: clinicopathologic features in fifteen cases. Int J GynecolPathol 1999; 18:63-68.
[Pubmed]
[7] Kobayashi Y, Murakami R, Sugizaki K, Yamamoto K, Sasaki S, Tajima N, Tajima H, Onda M, Kumazaki T: Primary leiomyoma of the ovary: a case report. Eur Radiol 1998;8:1444-6.[Pubmed]
[8] Emovon EU, Cahill DJ, Joels LA,
Stegmann MH: Bilateral primary ovarian leiomyoma: a rare cause of ovarian tumor in a young woman. J Obstet Gynecol 1999; 19:676 [Pubmed]
[9] Prayson RA, Hart WR: Primary smooth-muscle tumors of the ovary: a clinicopathologic study of four leiomyomas and two mitotically active leiomyomas. Arch Pathol Lab Med 1992; 116:1068-71.[Pubmed]
[10] Pandit MJ, Watson NR, Mackenzie IZ: Leiomyoma of the ovary. J Obstet Gynaecol 1997; 17:503-4.
[Pubmed]
[11] Lerwill MF, Sung R, Oliva E, Prat J, Young RH. Smooth muscle tumors of the ovary: a clinicopathologic study of 54 cases emphasizing prognostic criteria, histologic variants, and differential diagnosis. Am J Surg Pathol 2004;28:1436-51.
[Pubmed]
[12] Wellmann KF. Leiomyoma of the ovary: report of an unusual case and review of the literature. Can Med Assoc J 1961;85:429-32.[Pubmed]
[13] Rajabi P, Hani M, Bagheri M, Mirzadeh F. Large ovarian leiomyoma in young woman. Adv Biomed Res 2014 28;3:88.[Pubmed]
[PMC Fulltext]

