Original Article

Direct Immunofluorescence Study in Discoid Lupus Erythematosus
* Reema Bhushan, *Shilpi Agarwal, *Ram Chander, * Kiran Agarwal,
- *Department of Pathology, Lady Hardinge Medical
College, New Delhi, India
- Submitted: Monday, February 13, 2017
- Accepted: Monday, April 10, 2017
- Published:: Friday, April 28, 2017
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Diagnosis of a classical case of Discoid lupus erythematosus (DLE) is generally clinical. However, histopathological study of skin biopsy is helpful to confirm the diagnosis in early DLE lesions and in DLE variants. There is however paucity of large studies on its direct immunofluorescence (DIF) findings in India.
Patients and Methods
The study was conducted in the Department of Pathology on 34 clinically suspected cases of DLE who presented in the Department of Dermatology, Venereology &Leprosy at Smt. Sucheta Kriplani Hospital from 2012 to 2014.
Results
Histopathological diagnosis of DLE could be made in 30/34 (88.2%) cases while 4/34 (11.8%) cases showed non specific findings on histopathology. These four cases showed positive lupus band test on DIF examination, hence rendering the diagnosis of DLE. DIF was positive in 30/34 (85.3%) cases at the dermoepidermal junction (DEJ) in the form of lupus band test (LBT) in the lesional skin biopsy. The majority of cases showed deposit of multiple immunoreactants at DEJ (61.7% cases) with combined positivity for IgM plus IgG in 7/34 (20.6%) cases. Five cases (14.8%) cases in addition also showed DIF positivity in the dermal blood vessel (DBV) wall.
Conclusions
Direct immunofluorescence is a useful diagnostic technique in the diagnosis of DLE. However, it should be used in conjunction with histopathology.
Key Words
Direct immunofluorescence, Discoid lupus erythematosus, Lupus band test.
Introduction
Discoid lupus erythematosus (DLE) is a chronic dermatological disease that can lead to scarring, hair loss, and hyperpigmentation. Hence, early recognition and treatment is essential [1].
Although the diagnosis of classical DLE is generally clinical, histopathological study of skin biopsy is helpful to confirm the diagnosis in early DLE lesions and in DLE variants. The histopathological findings in DLE are well described, and there is a paucity of large studies on its direct immunofluorescence (DIF) findings in India [2]. Lupus band test (LBT) in the lesional skin is a very sensitive and specific test for DLE. Apppoximately 90-95% of the patients with discoid lupus erythematosus have positive LBT in the involved skin.
Lupus band test is considered positive when one or more immunoreactants (IgG, IgM, C3, and IgA) are found at the DEJ [3]. The purpose of this study was to analyze the direct immunofluorescence features in the cases of DLE, cases in which the clinical presentation of DLE was not classical, such as early DLE lesions, DLE variants and to correlate DIF findings with histopathology.
Material and Methods
The study was conducted from 2012 to 2014 in the Department of Pathology on 34 clinically suspected cases of Discoid lupus erythematosus presenting in the Department of Dermatology, Venereology& Leprosy at Smt. Sucheta Kriplani Hospital. A single 4 mm punch biopsy of skin lesion was taken & it was bisected. One half was sent for histopathological examination in 10% neutral formalin and other half in Michel’s medium (pH = 7.25) for direct immunofluorescence examination. Five µm thick tissue sections were cut for imunofluorescence study by a standardized method. Slides of each case was stained with fluorescein isothiocyanate (FITC) conjugated antibodies directed against IgG, IgM, IgA, C3 and fibrinogen and incubated in dark at 37°C for 1 hour.
After several washings in Phosphate buffer saline (PBS), the slides were mounted in glycerine PBS mixture and viewed under the immunofluorescence microscope fitted with an UV light source, under ideal excitation and barrier filter combination. Each slide was assessed for presence or absence of immunoreactants, type of immunoreactants, site of deposition, pattern and intensity of fluorescence. Final diagnosis of DLE was given after combining clinical findings, histopathology and DIF result. The approval of Ethics Committee of Lady Hardinge Medical College was obtained prior to the study. Informed consent from the participants was also obtained.
Results
The age of the patients ranged from 22-85 years with M:F =1:1.26. Final diagnosis of DLE (n=34/34) was given after combining histopathological and direct immunofluorescence features (100%). Histopatholgical diagnosis of DLE could be made in 30/34 (88.2%) cases while 4/34 (11.8%) cases showed non specific findings like focal basal cell vacuolization & perivascular inflammatory infiltrate. DIF examination in these four cases was positive in the form of lupus band test, hence suggesting the importance of using the direct immunofluorescence in conjunction with histopathology. DIF was positive in 29/34 (85.3%) cases at DEJ in the form of lupus band test. Multiple immunoreactants were seen in 21/34 (61.7%) cases. The cases showed a combined positivity for IgG plus IgM in 7/34 (20.6%) cases (Figure 1,&2). (Table 1) followed by IgG plus fibrinogen in 5/34 (14.7%) (Figure 3). However, the most common immunoreactant at DEJ was IgG (52.9 %). The most common pattern of deposit at DEJ was granular (24/29, 82.7%).(Table 2).
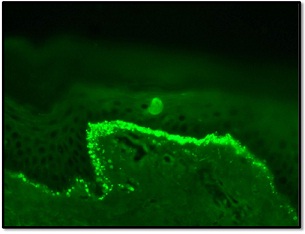
Figure 1: DIF of Discoid Lupus Erythematosus showing deposit of IgG in a linear granular pattern at basement membrane zone (Lupus band)
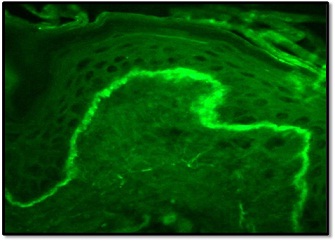
Figure 2: DIF of Discoid Lupus Erythematosus showing deposit of IgM in a linear granular pattern at basement membrane zone (Lupus band)
| |
Dermoepiermal Junction (DEJ) |
Blood Vessels (BV) |
| IgG,IgM |
7 |
0 |
| IgG,FIB |
5 |
0 |
| IgM |
4 |
0 |
| IgG, C3, FIB |
3 |
0 |
| IgM, FIB |
3 |
0 |
| FIB |
2 |
3 |
| IgM, C3 |
2 |
0 |
| IgG |
2 |
2 |
| IgG,IgM, C3, FIB |
1 |
0 |
| Negative |
5 |
29 |
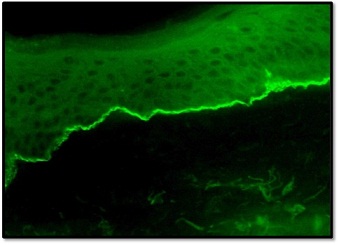
Figure 3: DIF of Discoid Lupus Erythematosus showing deposits of fibrinogen in a linear homogeneous pattern at basement membrane zone
| Site – pattern |
DLE |
Percentage (%) |
| DEJ – Granular |
21 |
72.4% |
| DEJ - Granular + DBV |
5 |
17.3% |
| DEJ - Granular +DEJ - Homogenous |
3 |
10.3% |
| Total |
29 |
100% |
In addition, 5/34 (14.8%) cases showed DIF positivity in dermal blood vessels (DBV) most commonly with fibrinogen in 3/34 (8.9%) cases followed by IgG in 2/34 (5.9%) cases. On histopathology, these cases showed superficial and deep dermal perivascular chronic inflammatory infiltrate. These cases also showed positive lupus band test hence aiding in the diagnosis of DLE. All the immunoreactants in DIF study showed strong immunofluorescence intensity. In the present study, 25/34 (73.5%) cases showed good histo-immunological correlation with positive DIF and characteristic histopathology.
Discussion
The age of patients in this study ranged from 22 years to 85 years (mean age 39.7 years) similar to Sandra et al., [4] who reported age range of 22 - 48 years (mean age 36.25 years). There was a slight female preponderance (M:F=0.78:1) which is in concordance with Kulthanan et al., [5] ( M:F = 0.75:1).
The definitive histopathological diagnosis of DLE was made in 30/34 (88.2%) cases which was consistent with observations of Minz et al., [6] &Naqqash et al., [7]
who reported a diagnostic histopathology in 82% &79.7% of DLE respectively.
Four cases showed non specific findings like focal basal cell vacuolization &perivascular inflammatory infiltrate. These cases showed positive LBT. Hence, DIF played a role in the diagnosis of these four cases in which histopathology with clinical findings were unable to make the definitive diagnosis.
In the present study, on DIF examination, 29/34 (85.3%) cases of DLE showed immunoreactant deposition in the form of lupus band test while 5/34 (14.7%) cases were negative. In these five cases, histopathological finding showed characteristic findings, hence rendering the diagnosis of DLE. Minz et al., [6] & Isfer et al., [8] and Bharti S et al., [2] found positive lupus band test at DEJ in 59%, 69% and 68% of DLE patients respectively. Sandra et al., [4] found that DIF was diagnostic in 100% cases. IgG was the most common immunoreactant seen at DEJ in 18/34 (52.9%) cases in this study, which is similar to the findings of Naqqash et al., [7], Kulthanan et al., 5, Al Swaid et al., [9], Bharti S et al., [2] & Beutner et al., [10]. However, Sandra et al., [4] & Isfer et al., [8] found IgM to be the predominant immunoreactant.(Table 3).
| DLE |
Kulthanan et al(1996) |
Sandra et al(1998) |
Isfer et al (1996) |
Naqqash et al(2011) |
Bharti S et al(2015) |
This study |
| Age |
15-68 yrs |
22-48yrs |
6-79 yrs |
14-60 yrs |
6-65yrs |
22-85 yrs |
| M:F |
0.75:1 |
0.23:1 |
0.4:1 |
0.2:1 |
0.66:1 |
0.78:1 |
| HPE |
100% |
100% |
100% |
79.7% |
60% |
88.2% |
| DIF |
90% |
100% |
69% |
79.3% |
68% |
85.3% |
| Multiple immunoreactant s at DEJ |
62% |
87.5% |
66.6% |
57.6% |
34% |
61.7% |
| MC @ DEJ |
IgG(57%) |
C3& IgM |
IgM(52.3%) |
IgG(74%) |
IgG(41.3%) |
IgG(52.9%) |
| DIF @DBV |
15% |
- |
6.9% |
- |
12% |
14.7% |
Deposit at the dermal blood vessels was an additional finding in the study. Five out of thirty four (14.7%) cases also showed DIF positivity in the DBV with fibrinogen in 3/34 (8.8%) cases and with IgG in 2/34(5.9%) cases. Kulthanan et al., [5] reported DIF positivity of 15% in the DBV with C3 (9%), IgM(5%) and IgG (2%) while Isfer et al., [8] reported 6.9% DIF positivity in the DBV with IgM (5%) and C3 (1.7%).
Immunoreactant deposits at blood vessel walls or sometimes a combination of deposits at the DEJ and immunofluorescence of vascular wall may occur in LE [5]. DIF positivity at the DEJ and at the DBV was strong in intensity in all the cases.
The quality of lupus band positivity can be affected by duration, distribution and type of lesions, sun exposure, prior steroid therapy, etc [7]. Some studies demonstrated that lesions of less than 3 months duration may not reveal immunoglobulin or complement deposition at DEJ [11]. This parameter could not be defined in our study as the duration of the lesions were not specified.
In the present study, the sensitivity of histopathology is not significantly greater than that of DIF (P value=1.000). However, histopathology gave positive or suggestive results in almost all the cases, in contrast to DIF that gave negative results in five patients. A combination of the two techniques yielded more reliable results (100%) than either technique alone (HPE=88.2%, DIF=85.3%). This signify the importance of using and incorporating the direct immunofluorescence findings of the skin biopsy in this study. The yield of combined sensitivity of both techniques together was greater than either of the two techniques separately. This is similar to the study by Nieboer [12]. DIF, thus helps in providing additional diagnostic information in the histopathologically equivocal cases.
Conclusion
Direct immunofluorescence is a useful diagnostic technique in the diagnosis of DLE. However, it should be used in conjunction with histopathology.
Authors' Contribution
RB: carried out the experiments and interpreted the results,
carried out the literature search and prepared the draft manuscript, designed
the study and performed the analysis, conceived the study, participated in
design and edited the final manuscript.
SA: interpreted the results, prepared the draft manuscript,
designed the study and performed the analysis, conceived the study, participated
in design and edited the final manuscript.
RC: conceived the study, participated in design and edited
the final manuscript
KA: participated in design and edited the final manuscript
Conflict of Interests
The authors declare that there are no conflicts of interests
Ethical Considerations
The study was approved by the Institute Ethics Committee and
written informed consent was obtained from each participant.
Funding
None declared
Acknowledgement
None
References
[1].Panjwani S. Early Diagnosis and
Treatment of Discoid Lupus Erythematosus. J Am Board Fam Med 2009; 22:206 –213.
[PubMed] [Full
text]
[2]. Bharti S, Dogra S, Saikia B, Walker R
M, Chhabra S, Saikia U N. Immunofluorescence profile of discoid lupus
erythematosus. Indian J Pathol Microbiol 2015; 58:479- 82. [PubMed]
[Full
text]
[3]. Mehta V, Sarda A, Balachandran C.
Lupus band test. Indian J Dermatol Venereol Leprol 2010; 76:298-300. [PubMed]
[Full
text]
[4]. Sandra A, Srinivas CR, Balachandran
C, Shenoi SD. Direct immunofluorescence in lesional and uninvolved skin in DLE.
Ind J Dermatol Venereol Leprol 1998; 64:150-152. [PubMed]
[Full
text]
[5]. Kulthanan K, Roongphiboolsopit P,
Chanjanakijskul S, Kullavanijaya P.Chronic Discoid Lupus Erythematosus in
Thailand: Direct Imnofluorescence Study. Int J Dermatol 1996; 35:711-714. [PubMed]
[6]. Minz RW, Chhabra S, Singh S, Radotra
BD, Kumar B. Direct immunofluorescence of skin biopsy: Perspective of an
immunopathologist. Ind J Dermatol Venereol Leprol 2010; 76:150-157. [PubMed]
[Full
text]
[7]. Naqqash S, Asad F, Pal SS. Direct immunofluorescence and Histopathology in chronic discoid lupus erythematosus. J Pak Asso Dermatol 2011; 21: 98-101.
[Full
text]
[8]. Isfer RS, Sanches JA, Neto CF, Cernea
SS, de Oliveira ZNP, Vilela MAC, Silva ML, Miyachi LM, Fukumori LMI, da Silva
SR. Direct immunofluorescence in Lupus Erythematosus (LE). Sao Paulo Med J 1996;
114(2):1141-1147. [PubMed]
[9].Al-Suwaid AR, Venkataram MN,
Bhushnurmath SR. Cutaneous lupus erythematosus: comparison of direct
immunofluorescence findings with histopathology. Int J Dermatol 1995;
34:480-482. [PubMed]
[10] Beutner E, Jablonska S, Kumar V.
Direct immunofluorescence in lupus erythematosus. In: Beutner E, Chorzelski TP,
Beau SF, eds. Immunopathology of Skin. New York: Wiley Medical Publication.
1987; p499-523.
[11]. Dahl MV. Usefulness of Direct
Immunofluorescence in Patients With Lupus Erythematosus. Arch Dermatol.
1983;119(12):1010-1017. [PubMed]
[12].Nieboer C. The reliability of
immunofluorescence and histopathology in the diagnosis of discoid lupus
erythematosus and lichen planus. Br J Dermatol 1987; 116: 189- 98. [PubMed]

