Original Article

A Study of Conjunctival Impression Cytology in Patients with Various Types of Psoriasis
Prakash Kumar1, Rajendra P. Maurya1, Prashant Bhushan1,Virendra P. Singh1, Mahendra K. Singh1, Sanjay Singh2, Rajendra S. Garbyal3, Mohan Kumar3
- 1Department of Ophthalmology, Institute of Medical Sciences, Banaras Hindu University, Varanasi-221 05 (U.P.) India
- 2Department of Dermatology & Venerology, Institute of Medical Sciences, Banaras Hindu University, Varanasi-221 05 (U.P.) India
- 3Department of Pathology, Institute of Medical Sciences, Banaras Hindu University, Varanasi-221 05 (U.P.) India
- Submitted: March 27, 2012;
- Accepted June 30, 2012
- Published: July 21, 2012
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective:
To evaluate the changes in specimens of conjunctival impression cytology specimens in patients suffering from various types of psoriasis.
Settings:
Departments of Ophthalmology, Pathology and Dermatology & Venerology, Institute of Medical Sciences, Banaras Hindu University, Varanasi (U.P.) INDIA.
Materials and Methods:
In this case control study, conjunctival impression cytology specimens were obtained from 29 psoriatic patients and 12 healthy controls without having any ocular abnormalities between November 2006 and May 2008. Specimens were graded on a scale of zero to three according to Nelson’s grading systems.
Results:
Out of 29 psoriatic patients, 82.3% had chronic plaque type, 10.3% had Erythrodermoid and 3.9% had pustular type of psoriasis. Conjunctival epithelial changes were observed in 23 (79.31%) patients (grade I changes in 41.4%, grade II in 27.6% and grade III changes in 20.7%). In the control group only 2(16.7%) cases had grade I changes while rest showed no epithelial changes. All cases of psoriatic erythroderma revealed worse cytological changes (grade III in 66% and grade II in 33.3% cases) while 29.2% of chronic plaque psoriasis and 50% of pustular psoriasis showed worse cytological changes. There was no significant correlation between duration of the disease and severity with cytological grading.
Conclusion:
Conjunctival impression cytology being a simple and non-invasive technique can be an important guideline in early diagnosis and treatment of ocular changes in psoriasis patients. As in our study, psoriatic erythroderma cases showed worse cytological changes (grade II
& III) than other types of psoriasis. Hence early intervention and referral of these types of psoriasis patients to ophthalmologists is essential.
Introduction
Psoriasis is a non-infectious, immunologically mediated, chronic recurrent inflammatory disease of the skin, with both genetic and environmental predisposing risk factors. Psoriastic lesions are characterized by well demarcated erythematous plaque, with silvery scales, occurring usually on the scalp, ears, genitalia, skin over the bony prominence and extensor surfaces. It affects 1 to 3% of the world population [1]. Psoriasis rarely involves the eyes. Ocular manifestations in patients with psoriasis have been observed in various studies [2-5]. The eyelids are frequently involved in psoriasis, the scaling process leading to madrosis, blepharitis, cicatrical ectropion and trichiasis [6]. Other ocular lesions reported are chronic non-specific conjunctivitis, keratitis, kerato-conjunctivitis sicca and uveitis [7-9], Tear film instability and Meibomian gland
dysfunction [10], dry eye and conjunctival surface disorders [11-12].
Conjunctival impression cytology is a fast, non-invasive, relatively easy to perform, reliable technique for study of ocular surface disorders [13]. The aim of this study is to determine the changes in surface epithelium of conjunctiva in various type of psoriasis.
Materials and methods
The study subjects included 29 patients with psoriasis who had mean age of 35.90 years with male female ratio of 1.9:1 and 12 healthy controls. Control eyes were those of patients without major ocular complaints and ocular surface abnormalities, having only refractive errors, who had mean age 30.75 with male:female ratio of 3:1.
The study was carried out in the Department of Ophthalmology jointly with Department of Pathology and Department of Dermatology
& Venerology, Institute of Medical Sciences, Banaras Hindu University, Varanasi (U.P.) India, for a period two years (2006-2008). Each study subject underwent detailed history taking including duration of the disease, previous therapy and eye complaints and detailed ocular examination including slit lamp examination to identify any ocular surface abnormalities or external eye diseases. The severity of psoriasis was determined by psoriasis area and severity index (PASI) in all patients.
Conjunctival impression cytology specimens were obtained from inter-palpebral temporal bulbar conjunctiva after topical anesthesia. A cellulose acetate filter paper (Millipore filter (HAWP02500) strip size 5 x 25 mm with a pore size of 0.45 was used. Cells adhering to the filter paper were immediately transferred to a glass slide which was stored in 95% ethanol at +4°C to prevent evaporation. Staining was done utilizing both PAP (Alcian Blue) and PAS (Periodic Acid Schiff) technique. Conjunctival impressions were graded according to classification of Nelson [14] on scale of 0 to 3.
Grade 0: The epithelial cells are small and round with eosinophilic staining cytoplasm.
The nuclei are large, basophilic, with a nucleo-cytoplasmic ratio of 1:2.
The goblet cells are abundent, plump and oval shaped having intensively PAS positive cytoplasm.
Grade I: The epithelial cells are slightly larger, more polygonal and have eosinophilic staining cytoplasm.
The nuclei are smaller with a nucleo-cytoplasmic ratio of 1:3. The goblet cells are less in number,
however they still maintain their plump oval shape, with an intensively PAS positive cytoplasm.
Grade II: The epithelial cells are larger and polygonal, occasionally multinucleated with variably staining cytoplasm.
The nuclei are small with a nucleo-cytoplasmic ratio of 1:4 to 1:5. The goblet cells are markedly
decreased in number and are smaller, less intensively PAS positive, with poorly defined cellular borders.
Grade III: The epithelial cells are large and polygonal with basophilic staining cytoplasm. The nuclei are small,
pyknotic and in many cells, completely absent. The nucleo-cytoplasmic ratio is greater than 1:6.
Goblet cells are completely absent.
Students-t test and chi-square test were performed to compare the scores of study subjects with the control group.
Results
Out of the 29 patients, 24 (82.3%) were of Chronic Plaque type, 3(10.3%) erythrodermoid type and 2 (3.9%) pustular type psoriasis (Fig. 1-3). Conjunctival epithelial changes were present in 23 (79.31%) patients which was statistically significant. 41.4% of total psoriatic patients showed grade I changes, 27.6% grade II, 20.7% (Table 1)
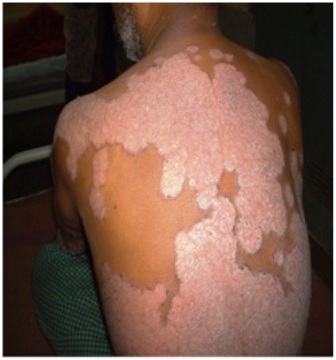

Figure-1: Patients of Chronic plaque psoriasis. Figure-2: Patients of psoriatic erythroderma
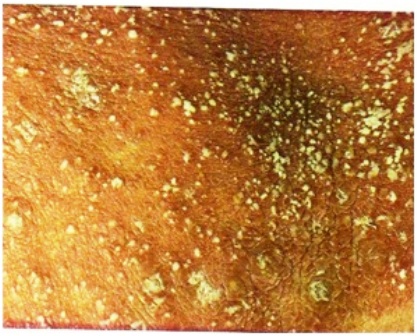
Figure-3: Pustular psoriasis.
Table-1 Comparison of cytological grading of patient and control group
| Cytological grade |
No. of patients |
% in patient |
No of control |
% in control |
|
0 |
6 |
20.7 |
10 |
83.3 |
|
I |
12 |
41.4 |
2 |
16.7 |
| II |
8 |
27.6 |
0 |
0 |
| III |
3 |
10.3 |
0 |
0 |
| Total |
29 |
00 |
12 |
100 |
While correlating between types of psoriasis and cytological grading the difference was statistically significant (χ2=14.605; p=0.002). Among the chronic plaque psoriasis 45.8% belonged to grade I, 25% to grade II and only 4.2% to grade III. 66.7% of psoriatic erythroderma belonged to grade III, 33.3% of grade II changes while none of the patients of psoriatic erythroderma were found of grade 0 and grade I. 50% of pustular psoriasis belonged to grade I and 50% of grade II changes [Table 2].
Table-2 Correlation between type of psoriasis and cytological grading
| Type of Psoriasis |
No.
(%) |
Cytological grades of conjunctival impression cytology |
|
|
Grade 0 |
% |
Grade I |
% |
Grade II |
% |
Grade III |
% |
Chronic Plaque
psoriasis |
24
(100%) |
6 |
25 |
11 |
45.8 |
6 |
25 |
1 |
4.2 |
Erythrodermoid
0psoriasis |
3
(100%) |
0 |
0 |
0 |
0 |
1 |
33.3 |
2 |
66.7 |
| Pustular psoriasis |
2
(100%) |
0 |
0 |
1 |
50 |
1 |
50 |
0 |
0 |
χ2 = 14.605; d.f=3; p=0.002
In this study, the minimum duration of disease was one year while maximum duration was 10 years (mean duration =5.05). There was no significant correlation between disease duration and cytological grading [Table 3]. Out of the 29 psoriatic patients, severity of 3 (10.3%) patients was less than 0.1 which belonged to grade 0 while 2 patients belonged to grade I. Severity of 15 (51.7%) patients were between 0.1-0.2 of which 4 belonged to grade 0, 7 to grade I
& 4 to grade II. Severities of 5 (17.2%) were between 0.2-0.3 of which one patient belonged to grade-1, 2 belonged to grade II and 2 belonged to grade III. Severities of 3 patients were between 0.3-0.4 while severities of 3 patients were more than 0.4 [Table 4]. No significant correlation was found between severity of disease and conjunctival impression cytological grading (χ2=12.728; p=0.389). 16(55.2%) patients belonged to PASI score less than 10 and remaining 13(44.8%) belonged to PASI score between 20-30. No significant correlation was found between PASI value and impression cytological grade (χ2=11.907; p=0.064).
Table-3 Correlation between Disease duration and impression cytology, grading
Disease
duration
(years) |
Total |
Conjunctival impression cytology grade |
|
|
|
Grade o |
Grade I |
Grade II |
Grade III |
|
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
| 0-3 |
9 |
31.0 |
4 |
66.7 |
3 |
25.0 |
1 |
12.5 |
1 |
33.3 |
| 3-6 |
10 |
34.5 |
2 |
33.3 |
6 |
50.0 |
2 |
25 |
0 |
0 |
| 6-9 |
5 |
17.2 |
0 |
0 |
2 |
16.7 |
2 |
25 |
1 |
33.3 |
| >9 |
5 |
17.2 |
0 |
0 |
1 |
8.3 |
3 |
37.5 |
1 |
33.3 |
| Total |
29 |
100 |
6 |
100 |
12 |
100 |
8 |
100 |
3 |
100 |
χ2 = 11.278; d.f=1; p=0.257
Table-4 Conjunctival impression cytological grading according to severity of disease
Overall
severity
of
disease |
Total |
Conjunctival impression cytology grading |
|
|
|
Grade o |
Grade I |
Grade II |
Grade III |
|
No |
% |
No |
% |
No |
% |
No |
% |
No |
% |
| <0.1 |
3 |
10.3 |
1 |
16.7 |
2 |
16.7 |
0 |
0 |
0 |
0 |
| 0.1-0.2 |
15 |
51.7 |
4 |
66.7 |
7 |
58.3 |
4 |
50.0 |
0 |
0 |
| 0.2-0.3 |
5 |
17.2 |
0 |
0 |
1 |
8.3 |
2 |
25.0 |
2 |
66.7 |
| 0.3-0.4 |
3 |
10.3 |
0 |
0 |
1 |
8.3 |
1 |
12.5 |
1 |
33.3 |
| >0.4 |
3 |
10.3 |
1 |
16.7 |
1 |
8.3 |
1 |
15.5 |
0 |
0 |
| Total |
29 |
100 |
6 |
100 |
12 |
100 |
8 |
100 |
3 |
100 |
χ 2 = 12.728; d.f=12; p=0.389
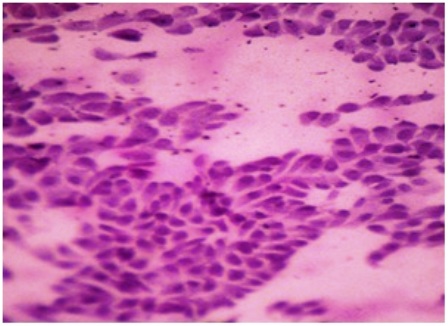
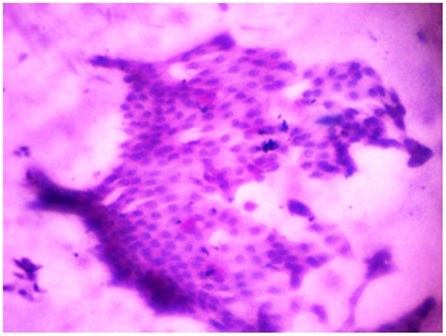
An important finding in this study was that some of the cases showed high grade squamous epithelial changes (corresponding to grade III) without a corresponding depletion in goblet cells. Tall columnar or signet ring like goblet cells with nuclear hyper-chromasia was observed in fair number against a background of discohesive squamous cells of low nucleocytoplasmic ratio [Figure 4-8].
a
![Figure-4: Photomicrograph of grade-0 changes in CIC showing (a) sheets of epithelial cells in cohesive fashion with round to oval nuclei & moderate amount of cytoplasm (PAP x 40). (b) Sheets of epithelial cells with fare number of goblet cells (pink blots) [PAS x 40].](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img4a.jpg)
![Figure-4: Photomicrograph of grade-0 changes in CIC showing (a) sheets of epithelial cells in cohesive fashion with round to oval nuclei & moderate amount of cytoplasm (PAP x 40). (b) Sheets of epithelial cells with fare number of goblet cells (pink blots) [PAS x 40].](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img4b.jpg)
b
Figure-4: Photomicrograph of grade-0 changes in CIC showing (a) sheets of epithelial cells in cohesive fashion with round to oval nuclei
& moderate amount of cytoplasm (PAP x 40). (b) Sheets of epithelial cells with fare number of goblet cells (pink blots) [PAS x 40].
a
![Figure-5: Photomicrograph of grade-I changes in CIC, showing (a) sheets of cells with ample amount of cytoplasm and relatively smaller nuclei size (PAP x 40); (b) sheets of epithelial cells with fair number of goblet cells (pink blots)[PAS x 40]](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img5a.jpg)
![Figure-5: Photomicrograph of grade-I changes in CIC, showing (a) sheets of cells with ample amount of cytoplasm and relatively smaller nuclei size (PAP x 40); (b) sheets of epithelial cells with fair number of goblet cells (pink blots)[PAS x 40]](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img5b.jpg)
b
Figure-5: Photomicrograph of grade-I changes in CIC, showing (a) sheets of cells with ample amount of cytoplasm and relatively smaller nuclei size (PAP x 40); (b) sheets of epithelial cells with fair number of goblet cells (pink blots)[PAS x 40]
a
b
Figure-6: Photomicrograph of grade-II changes in CIC, showing (a) sheets & isolated form of cells with reduced nucleocytoplasmic ratio
& focal squamous cell metaplasia (PAP x 100); (b) sheets of epithelial cells with scanty goblet cells and evidence of focal squamous metaplasia (PAS x 40).
a
![Figure-7: Photomicrograph of grade-III changes in CIC, showing (a) squamous metaplasia and very occasional clumps of cohesive epithelial cells with round to oval nuclei. (→) [PAP x 40] (b) squamous metaplasia in complete absence of goblet cells. (PAS x 100)](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img7a.jpg)
![Figure-7: Photomicrograph of grade-III changes in CIC, showing (a) squamous metaplasia and very occasional clumps of cohesive epithelial cells with round to oval nuclei. (→) [PAP x 40] (b) squamous metaplasia in complete absence of goblet cells. (PAS x 100)](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img7b.jpg)
b
Figure-7: Photomicrograph of grade-III changes in CIC, showing (a) squamous metaplasia and very occasional clumps of cohesive epithelial cells with round to oval nuclei. (→) [PAP x 40] (b) squamous metaplasia in complete absence of goblet cells. (PAS x 100)
a
![Figure-8: Photomicrograph showing (a) discohesive epithelial cells in marked mucous mixed background with endocervical like morphology (eccentrically nucleus with tall columnar like cytoplasm) [PAP x 40] (b) signet ring cell formation due to mucinous secretion in cytoplasm (→).](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img8a.jpg)
![Figure-8: Photomicrograph showing (a) discohesive epithelial cells in marked mucous mixed background with endocervical like morphology (eccentrically nucleus with tall columnar like cytoplasm) [PAP x 40] (b) signet ring cell formation due to mucinous secretion in cytoplasm (→).](/manuscripts/EYEXNIHPFG/0/imgfolder/wjp_11_img8b.jpg)
b
Figure-8: Photomicrograph showing (a) discohesive epithelial cells in marked mucous mixed background with endocervical like morphology (eccentrically nucleus with tall columnar like cytoplasm) [PAP x 40] (b) signet ring cell formation due to mucinous secretion in cytoplasm (→).
Discussion
Psoriasis is a chronic, recurrent, inflammatory cutaneous eruption, characterized by well defined erythematous silvery scaled plaques. Inflammatory process may involve the ocular surface epithelium and cause altered vascularization and scar formation. Tseng
et al. (1985) stated that the pathogenesis of squamous metaplasia of ocular surface epithelia may be due to loss of vascularization and scar formation 13. In our study, conjunctival impression cytology specimens were taken from various types of psoriasis to determine the epithelial cell morphology, nucleo-cytoplasmic characteristics, goblet cell density etc.
In this study, out of 29 psoriatic patients, 23(79.3%) had cytological changes while in control group only 2(16.7%) had cytological changes. The difference was statistically significant between the study and control group (p<0.001). Among the psoriatic patients, 41.4% showed grade I cytological changes, 27% grade II and 10.3% grade III while in 20.7% cases grade 0 changes were observed. In a similar study done by Karbulut AA
et al. (1999) 11 in fifty psoriatic patients, 50% had grade 0, 30% had a grade I and 20% had a grade II cytological changes.
As compared to Karbulut et al., study where maximum number of psoriatic patients (50%) had grade 0 changes while in our study maximum patients (41.4%) had grade I changes. In Karbulut et al., study none of the patients showed grade III changes as compared to our study where 10.3% patients had grade III changes. The difference may be due to presence of psoriatic erythroderma cases (10.34%) out of total patients in our study. While in Karbulut
et al., study all psoriatic patients belonged to plaque type. Another study conducted by Soker Sevda
et al., [6] (2008) on 64 eyes of 32 patients of chronic plaque type psoriasis, grade 0 changes was observed in 39%, grade I in 36% and grade II changes in 25% eyes. None of his patients showed grade III changes.
In our study, a comparision of psoriatic type and cytological grading, revealed that out of 3 patients of psoriatic erythroderma, 2(66.7%) showed grade III changes and one (33.3%) had grade II changes, while in chronic plaque type psoriasis, only 4.2% patient had grade III changes. The difference was statistically significant (P<00.5). This indicates that there was worsening of cytological grading in psoriasis patients other than chronic plaque type.
In this study, there was no statistical significance in terms of impression cytology grading versus duration of disease or overall severity/PASI score in patient with psoriasis. This finding was supported by Karbulut
et al., [11] and Soker Sevda et al., [6]. Thus it may be concluded that squamous metaplasia is associated with primary inflammatory process of psoriasis rather than complication of disease or side effect of treatment [6]. Higher incidence of cytological changes in our study as compared to previous study can be the result of smaller study group and needs to be verified in a larger study particularly on psoriatic erythroderma cases.
Conclusion
As Psoriatic erythroderma cases showed worse cytological changes (grade III & II) than other type of psoriasis so these types of psoriatic patients should be referred to ophthalmologists for early evaluation and intervention. Impression cytology can be a guideline in early management of ocular changes in psoriasis.
Authors’ Contribution
PK : Performed the literature search carried out the study and prepared the draft manuscript.
RPM: Carried out the literature search and designed the study under guidance.
VPS: collected analyzed and interpreted the clinical data
MKS: designed the study and interpreted the results, he also revised the manuscript
PB: interpretation of data and revision of manuscript
SS: Designed the dermatological part of study and reviewed the final manuscript.
RSG: Collection evaluation and interpretation of pathological data
MK: collection and interpretation of pathological data and design of the study.
All authors read and approved the manuscript for publications
Ethical Considerations:
The study was approved by the ethics committee.
Conflict of interest
The authors declare that there are no conflicts of interests
References
[1]. de Lima FB, Abalem MF, Ruiz DG, Gomes Bde A, de Azevedo MN, Moraes HV Jr, Yeskel AS, Kara-Junior N. Prevalence of eye disease in Brazilian patients with psoriatic arthritis. Clinics (Sao Paulo). 2012; 67(3): 249-53.[Pubmed]
[2]. Sandvig K, Westerberg P. Ocular findings in psoriatics. Acta Ophthalmol (Copenh]. 1955; 33(4): 463-7.[Pubmed]
[3]. Knox DL. Psoriasis and intraocular inflammations. Trans Am Ophthalmol Soc. 1979; 77: 210-24.[Pubmed],[Full Text]
[4]. Lambert JR. Wright V. Eye inflammation in psoriatic arthritis. Ann Rheum Dis. 1976; 35(4): 354-6.[Pubmed]
[5]. Catsarou-catsari A, Katsambas A. Theodorpoulos P, Stratigos J. Ophthalmolgocal manifestations in patients with psoriasis. Acta Derm Venereol. 1984; 64(6): 557-9.[Pubmed]
[6]. Soker S, Nergiz Y, Cakmak S, Bahceci S, Aytekin S. The demonstration of changes in bulbar conjunctiva surface epithelium in the psoriatic patients treated with PUVA. Ann Ophthalmol. 2008; 40(2): 94-98.[Pubmed]
[7]. Whitemore PV. Skin and mucous membrane disorder. Vol. 5, In. Duane TD, Henkind P, Gold D. eds. Textbook of ophthalmology Philadelphia, Harper & Row, 1986.
[8]. Durrani K, Foster CS. Posterior Uveitis; a distinct clinical entity. Am J Ophthalmol. 2005; 139: 106-11.[Pubmed]
[9]. Paiva ES, Macaluso DC, Edwards A, Rosenbaum JT. Characterization of uveitis in patients with psoriatic arthritis. Ann Rheum Dis. 2000; 59(1); 67-70.[Pubmed]
[10]. Zengin N, Tol H, Balevi S, Gündüz K, Okudan S, Endoğru H. Tear film and meibomian gland functions in psoriasis. Acta Ophthalmol Scand. 1996; 74(4): 358-60. [Pubmed]
[11]. Karabulut AA, Yalvac IS, Vahaboghu H, Nurozler AB, Duman S. Conjunctival impression cytology and tear film changes in patients with psoriasis. Cornea. 1999; 18(5): 544-8.[Pubmed]
[12]. Erbagci I, Erbagci Z, Gungor K, Bekir N. Ocular anterior segment pathologies and tear film changes in patients with psoriasis vulgaris. Acta Med Okayama 2003; 57(6): 299-303.[Pubmed]
[13]. Tseng SC, Hirst LW, Maumenee AE, Kenyon KR, Sun TT, Green WR. Possible mechanism for loss of goblet cells in mucin deficient disorder. Ophthalmology. 1985; 91: 545-52.[Pubmed]
[14]. Nelson JD, Havener VR, Cameron JD. Cellulose acetate impressions of the ocular surface. Dry eye states. Arch Ophthalmol. 1983; 101(12): 1869-72.[Pubmed]

