Original Article

Effectiveness of Multicultural Communication between Radiographers and Patients and Its Impact on Outcome of Examinations
*William K. Antwi, *Kofi Adesi Kyei, *Lily N. A. Quarcoopome
*University of Ghana, College of Health Sciences, P.O. Box KB 369, Korle-Bu, Accra, Ghana
- Submitted Sunday, June 08, 2014
- Accepted:Friday, July 25, 2014
- Published Sunday, August 03, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
Communication plays an important role in the practice of radiography. It is important that radiographers are aware of patients’ physical and emotional needs which could be achieved through effective communication. The diversity of the patient population creates challenges to quality healthcare provision to all segments of the population, without effective communication.
Aim
The research aims at assessing the effectiveness of multicultural communication and its impact on the outcome of radiological examinations.
Method
A research design using quantitative approach was employed. A convenience sampling method was used to select a sample of 100 patients and 28 radiographers. A questionnaire consisting of close- and open-ended questionnaires were administered to the participants.
Results
The results showed that 39% (n = 11/28) radiographers were relatively fluent in other languages in addition to English. Also, radiographers employed other methods such as touch, hand gestures and sign language to overcome language barriers.
Moreover, 77% (n = 77/100) of the patients were fluent in English, though majority preferred communicating in their native languages. Nonetheless, 63% (n = 63/100) of the patients could not freely discuss their concerns with the radiographer and felt that the radiographer was not approachable. However, the patients had an overall good perception of the radiographer.
Conclusion
Generally, multicultural communication in the radiology department is effective. However, efforts are impeded due to time constraints and lack of guidelines to approach cultural barriers.
Key Words
Multicultural communication, radiography, verbal and non-verbal communication
Introduction
Communication plays an important role in the practice of radiography. In many countries, an important challenge to health care is the provision of services to a population that is culturally diverse with different languages [1]. Like their other counterparts in healthcare, radiographers provide services to a very diverse patient population in Ghana. The radiographer provides caring services to meet the needs of a diversity of patients while producing high quality radiographs [2]
Radiography generally involves communication in disseminating information to the patient by explaining the procedures and other related issues concerning the examination which involves a number of factors including patient interaction to result in quality diagnostic information [2] Emphasis is also placed on radiographers remaining sensitive to the physical and emotional needs of the patient through good communication along with other factors, while ensuring that the instructions and questions to the patient are clearly understood [2].
Multicultural communication in health care refers to translating patient education in the health care setting where many cultures are identified. Patient diversity, cultural context and communications are identified as factors that influence health care and patient response [3]. In countries like Ghana, the demand for culturally competent health care is the result of failure of the health care system to provide adequate care to all segments of the population, which is suggestive that understanding patient-provider communication is essential for development of policies for a competent health care system [4].
Booth (2008) identifies radiographer-patient relationship to consist of patient-centered and practitioner-centered approaches with a preference for the patient–centered approach [5]. Using this approach requires that the patient’s language and cultural background are considered during communication with the patient
Communication in medical imaging has not been fully explored by research despite its importance in interacting with patients in order to achieve quality diagnostic image [6]. Galanti (2000) suggests that many health professionals think that according the patient with respect may resolve most cultural problems. Multicultural communication is a complex issue and should therefore be effectively handled in order to ensure that patients are well-informed regarding procedures and their welfare [7].
For a collaborative radiographer-patient communication, multicultural communication may be given priority and may enhance outcome of diagnostic imaging procedures [8] and may consequently increase patient’s satisfaction.
The diversity of patients in the hospital setting creates a challenge of how to provide quality care to patients who may speak different languages and come from different cultural backgrounds [9]. Moreover, Heistad (2007) recognized that good communication is the key to both patient interaction and provision of quality diagnoses. Hampers et al. (1999) argue that although research has proven that language barriers are undesirable, it is unclear the effect the language barrier might have on the practice of the radiographer [10].
A study by Scott (2007) has identified various means of tackling language barriers such as acquiring knowledge about the prevalent cultural vocabulary, cultural and linguistic training and the use of evidence-based practice to improve the quality of care [8]. However, due to limited research to explore communication in multicultural settings, there is inadequate information on guidelines to follow in order to tackle cultural challenges and their potential impact on healthcare services, especially in Ghana.
The study aims to assess effectiveness of multicultural communication and their impact on the outcome of radiological examinations.
Objectives
To assess if communication barriers exist within the imaging unit of the study site
To assess radiographers knowledge about challenges of communication as regards to language barriers.
To identify skills, techniques and strategies adopted by radiographers
to overcome language and cultural barriers.
To determine if diagnostic information is compromised due
to the radiographer’s approach.
Methodology
A quantitative research design with a descriptive approach was used due to the nature of the study. This allowed the researcher to consider the phenomenon of interest from different perspectives and to develop a more holistic approach to communication in a multicultural environment [11]. The study was carried out at the Radiology Department of the Korle-Bu Teaching Hospital and the Korle-Bu Polyclinic. All qualified diagnostic radiographers in the Unit of the Hospital were the target group. Out-patients undergoing both general and special examinations were also recruited for the study. In all, 34 qualified radiographers at the radiology units were involved and 100 patient participants between the ages of 18 and 60 who are mentally sound were selected for the study using convenience sampling method. Student and intern radiographers as well as out-patients below the age of 18 and above the age of 60 undergoing imaging examination were excluded from the study.
Both closed- and open-ended questionnaires were used with one designed for radiographers and the other for patients. The questionnaires for the radiographers were sub-divided into three sections; A, B and C. Section A sought to collect radiographer’s demographic data, Section B assessed the working environment and section C assessed communication with patients and impact on the examination.
The questionnaire for patients however assessed patient’s communication skills and that with the radiographers. For the qualitative section, interviews and observation were tools used for the data collection. Interview (made of semi-structured questionnaires) and observation provided more insight to the study. The questionnaires were self-administered except for cases where the patients were illiterate in which case; they were administered by the researcher with the help of a relative. The data was collected over a period of four weeks.
Data collected was analyzed using Statistical Package for Social Science (SPSS) software (version 16.0) and Microsoft Excel 2007. The results were presented in tables, graphs and charts. Approval was obtained from the Ethical Review and Protocol Committee of the School of Allied Health Sciences. Approval for the study was obtained from the research ethics committee of a higher education institution. The ethics approval was supported by written permission for the study to be conducted at the study site with the ethical standard of confidentiality being upheld. All study participants gave informed consent prior to the commencement of the study and each data collection activity.
Results
In all 32 radiographers were targeted but 28 responded to the study constituting a response rate of 87.5%. However, all 100 patients successfully participated in the study. Out of the 28 radiographers, 20 were males and 8 were females with majority (58%) between the ages of 21-30 years. For the patients , 30% were 50+ years , 18% were between 41-50 years, 24% were between 31-40 years, 18% were between 20-30 years and the rest <20years. 60% were females where as 40% were males.
The results show that 46% of the radiographers were Akan with the least of them (4%) from the Krobo/Guan tribes. For the patients, 37% were Akans, followed by Ga/Damgbe (28%). Half of the radiographers (50%) have been working for more than five years, with only 5% in their first year of practice. Majority of the participants (50%) had been in the practice for five years and above (Figure.1).Majority (75%) of the radiographers said they attended up to 30 patients daily (Figure. 2). Majority of the radiographers (43%) stated they spend approximately 5-10 minutes on each patient, whereas 22% indicated 11-20 minutes and Table 1 shows that, patient’s co-operation and condition mostly influenced the time spent with a patient.
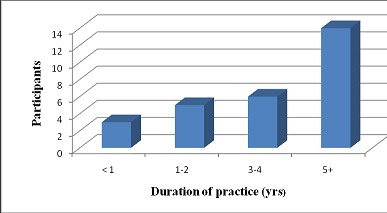
Figure 1: Duration of practice (in years), (n =28)
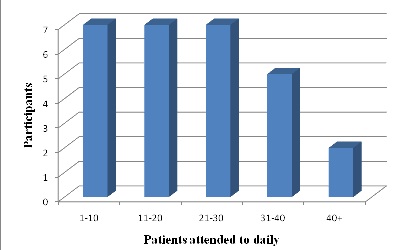
Figure 2: Patients attended to daily, (n=28)
|
|
Participants
|
Percent
|
|
Equipment condition
|
6
|
12
|
|
Medical examination involved
|
10
|
20
|
|
Patient's co-operation & condition
|
13
|
28
|
|
Availability of materials
|
4
|
8
|
|
Preventing unnecessary x-ray exposure
|
3
|
6
|
|
Procedure's explanation with good communication
|
8
|
16
|
|
Patient positioning
|
2
|
4
|
|
Evaluation/Planning
|
3
|
6
|
|
|
|
100
|
From the study, 39% of the radiographers could speak three or more languages apart from English, however, 53% of the patients indicated their level understanding when communicated to in English by the radiographers (Figure. 3) 79% indicated that they encountered barriers and challenges in communicating and resorted to other means such as sign languages, interpreter, hand gestures etc (Table 2) However, 75% of the radiographers encountered difficulties with patients due to language barriers resulting in some compromising results in (Figure. 4)
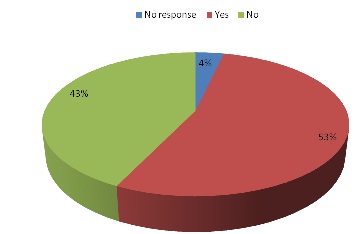
Figure 3: Ability of patient to understand radiographers in English, (n = 28)
|
Means of communication
|
Frequency
|
Percent
|
|
Sign language
|
15
|
54
|
|
Hand gesture
|
4
|
14
|
|
Call for interpreter
|
1
|
4
|
|
Hand gesture and sign language
|
2
|
7
|
|
Sign language and Touch
|
1
|
4
|
|
Sign language and call for an interpreter
|
1
|
4
|
|
No response
|
4
|
14
|
|
Total
|
28
|
100
|
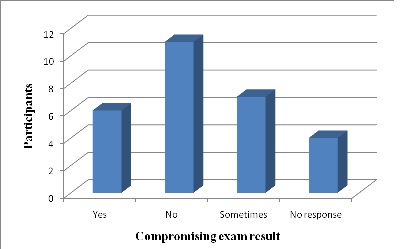
Figure 4: Examination results compromised due to language barriers, (n =28)
The results shows that 54% of the patients had prior information of the procedure(Figure. 5) where as 70% of the patients were visiting the radiology department for an examination for the first time.(Figure. 6)illustrated languages used in the procedure and English were dominant, followed by Twi but majority of patients preferred Twi for their communication (Figure. 7). 63% of patients did not ak questions or explanations during examination, and 63% of the patients also indicated that radiographers were not approachable (Figure. 8). When asked about their view on the radiographers, 24% stated that they were professional whiles 20% said they were friendly (Figure. 9) Majority of the patients (28%) rated communication with the radiographer as good and almost 50% rated the quality of service at the X-ray department as good(Figure. 10).
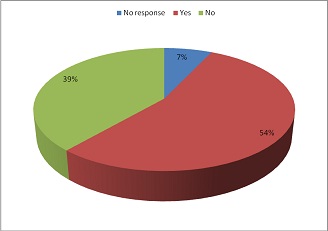
Figure 5: Explanation of exam before the procedure, (n=100).
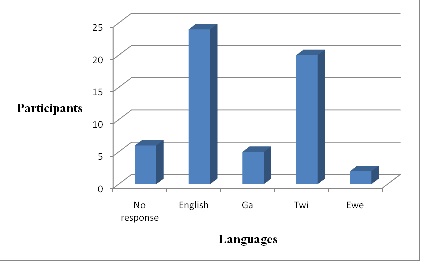
Figure 6: Language preference of patients during communication, (n=100).
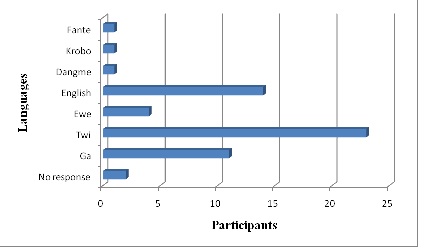
Figure 7: Languages spoken by participants, (n=100).
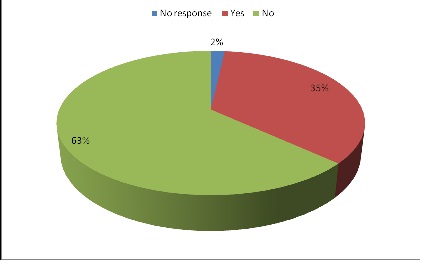
Figure 8: Approachable attitude of radiographer, (n=100)
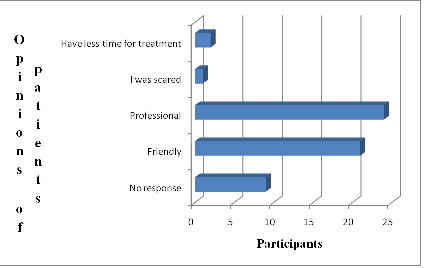
Figure 9: Patient’s view about the radiographer, (n =100)
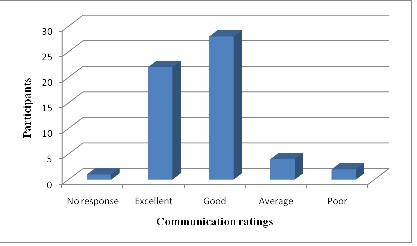
Figure 10: Rating communication with the radiographer, (n=100).
Discussion
Majority of radiographers (46%) were from the Akan speaking tribe with the minority from the Krobo and Guan tribes. This is a reflection of the distribution of tribes in Ghana which has the majority of the population coming from the Akan speaking tribe. The same pattern was recorded for patients. As demonstrated, 46% (n = 13/28) of the radiographers worked up to 6 hours daily where as a good number of them (43%) indicated working 8 hours a day. This is an indication of the long working hours of radiographers, although most participants 50% (n =14/28) considered their working environment to be conducive. This may be indicative that most radiographers had developed coping mechanisms to effectively manage their working environment and the resources available to them.
A good number of staff participants (75%) indicated attending to up to 30 patients. Furthermore, Figure 2, demonstrated that most respondents 43% (n =12/28) spent approximately 5-10 minutes on each patient. The large number of these patients that were attended to daily by radiographers may account for the limited time spent on each patient which is a major challenge in the Radiology Department [12]. Research has emphasized that for communication to be effective, the patient should feel that enough time is available for speaking and listening which would increase their overall satisfaction with the service [13].
From Table 1 , other factors influencing time spent with patients were outlined with the most being patient’s co-operation and condition (28%) as well as procedure’s used in the explanation with good communication (16%). This indicates that lack of good communication compromises the quality of healthcare delivery and the entire diagnostic process as already suggested by Schyve (2007) [14].
Communication and Its Impact on Examination
Thirty nine percent of the radiographers at the time of the study spoke three or more languages other than English. Furthermore, the distribution of the languages spoken by radiographers apart from English range from Twi, Ga and and Ewe. This reveals that most of the radiographers speak the major languages in Ghana namely Ga, Twi and Ewe while other Ghanaian languages such as Krobo, Adangme and international languages like French and Spanish are in the minority. This appears to be contrary to the need for radiographers to have minimum proficiency in a variety of languages and behaviours of patients to offer competent care [8].
Research has emphasized that for a more patient-centered approach, communication should be skewed towards the patient’s needs and preferences [15].
From the results, 53% of patients understood when radiographers communicated with them in English which was in line with a large percentage of the patient population. Seventy nine percent of the participants agreed that they encountered language barriers and this may be due to the changing demographics of the population due to rural-urban migration and the influx of other nationals into the country. These language barriers were encountered several times within 3the week by almost 32% of participants.
results from Table 2 outline other means of communication employed by radiographers when they encounter language barriers. It has been identified that communication is both verbal and non-verbal and is mainly through body language and tone of voice with less emphasis on the actual word content [16]. Hence other methods like touch, hand gestures and interpreters employed by the radiographers were expected. Surprisingly, very few radiographers resorted to using interpreters though it has been recommended [8]. Other skills, verbal and non-verbal communication styles have also been outlined by Canado and Garcia (2007) to enable radiographers to provide more competent care [17]. However, some of these skills and styles did not reflect in the results due to a different cultural environment or lack of knowledge about them.
The staff participants agreed that they encountered language difficulties because of language barriers. Accordingly, language barriers have been identified as a source of workplace stress for health care professionals [18]. However, it is important that radiographers communicate effectively with the patients as they are responsible for taking patient histories and providing instructions for pre and post procedural care to ensure patient safety at all times and achieve the desired diagnostic information [8].
Further, 30% of the respondents agreed that the results of the examination were not compromised due to language barriers. Additionally, some respondents retorted positively and indicated that language barriers could cause errors in the diagnostic process as mentioned by [19]. However, it is discriminatory for patients not to receive the same quality of care simply on the basis of language or ethnicity [8]. Radiographers may have to consider acquiring the ability to work effectively with patients from different cultures to eliminate this bias.
Patient’s Communication Skills
Most patients (70%) were first time visitors of the Radiology Department and additionally, 54% agreed that they had prior explanation of the procedure. This was a positive trend that was seen in the study and should be continued, though few of patients (18%) indicated that explanations were given by radiographers. The reason may be that most patients at the time of study were not familiar with the various categories of health professionals in the hospitals or radiology department. Subsequently, it could lead to situations where patients may not know who to direct their questions to and could cause the patient to lack adequate information about the procedures.
It was later indicated that 77% of the patients were fluent in English which was notably higher than the earlier observation recorded by 53% of radiographers. It could be inferred from this observation that the patients may be unfamiliar with some terminology used by the radiographers hence, creating ambiguity when instructions are given.
Results from Table 2demonstrated that majority of the patients spoke a combination of Ga, Twi and Ewe. Consequently, 23% which represents the majority of patients preferred Twi when communicating. Contrary to this, 24% responded that explanations about the procedure were given in English. This indication results in the need for radiographers to acquire and utilize basic vocabulary in local languages when communicating with patients [8] and be able to accurately predict when to do this.
Patient’s Opinion of Radiographers Communication Skills
Justifiably, 63% of patients asked questions and explanations of information they did not understand during the procedure, the same percentage of patients indicated that the radiographers did not have an approachable attitude. Contrary to this observation, it is required that radiographers demonstrate approachable attitude so patients could ask for explanation for information they do not understand for communication to be effective (Wilson, et al., 2009). Canado and Garcia (2007) have outlined skills to achieve this in their paper so that the radiographer may appear less unapproachable and effective communication could be realized.
The opinions of patients about the radiographer showed a positive trend and overall, more than 55% of participants rated communication with the radiographer as excellent and good(Figure. 10)and over 50% also rated the quality of service in the radiology department as excellent and good. This suggested that more than half of the clients seen showed an overall satisfaction with service in the department. It also appears to run concurrently with the study by [20] that good communication contributes to patient’s perception of high quality care and patients’ satisfaction.
Conclusion
The results of the study indicated that majority of radiographers in Ghana have good communication skills and are able to adapt to different situations by trying different approaches till the desired outcome is achieved. Generally, the study showed effective multicultural communication though further research needs to be done to identify existing communication skills, implement skills and guidelines that are absent.
Conflict of Interests
The authors declare that there is no conflict of interest
Authors’ Contribution
LQ and KAK, carried out the literature and prepared the draft manuscript
,KAK, and WKA carried out the experiment and VV interpreted the results
LQ and WKA designed the study and performed the analyses
KAK and WKA conceived the study and participated in the study design and
KAK edited the final manuscript
All authors read the script carefully and approved the final manuscript for submission
Funding
None
Ethical Considerations
The study was approved by the institute ethics committee.
Acknowledgement
None
References
[1].Klein, G.O. and Kajber, K. (2009). E-health tools For Patients and Professionals in a Multicultural World, In: European Federation for Medical Information, Stockholm: IOS Press.[pubmed]
[2].Adams HO. Effectiveness of communication between radiographers and patients and its impact on practice. University of Ghana 2009, Legon.
[3].Jan CS, Nardi DA. Asian Radiology Nursing with the Population. Radiology Nursing Journal, 2005; 24: 79-84.
[4]DeVoe JE, Wallace LS, Fryer GE Jr. Measuring patients' perceptions of communication with healthcare providers: do differences in demographic and socioeconomic characteristics matter? Health Expect. 2009 Mar;12(1):70-80. doi: 10.1111/j.1369-7625.2008.00516.x. [pubmed]
[5].Booth LA. The Radiographer-Patient Relationship: Enhancing understanding using a transactional analysis approach. Radiography 2008; 14: 323-331.
[6].Booth LA, Manning DJ. Observations of radiographer communication: An exploratory study using transactional analysis, Radiography, 2003; 12(4): 276-282.
[7].Galanti GA. An introduction to cultural differences. Western Journal of Medicine, 2000; 172 (5): 335-336 [pubmed]
[8].Scott A. (). Improving Communication for Better Patient Care. Radiol Technol. 2007 Jan-Feb;78(3):205-18; quiz 219-21..[pubmed]
[9].Heistad K. Tackling Cross-Cultural Communication Challenges in Health Care. http://www.culturecoach.biz/Resources/Tackling%20Cross%20Cultural%20in%20.pdf [Last accessed on September 6, 2014]
[10].Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999 Jun;103(6 Pt 1):1253-6.[pubmed]
[11].Collette C. Nursing and Health Care Research; A Skills-based Introduction. Prentice Hall International 1997, London
[12].Worrel J, Lee F. Cultural competence in diagnostic imaging. Academic Radiology, 2005; 12(2):232-236.[pubmed]
[13].Lee SM. A review of Language and Other Communication Barriers in Health Care. Washington, D.C.: Office of Minority Health, Department of Health and Human Services http://faculty.ksu.edu.sa/71640/Publications/COURSES/446%20CHS%20Communication%20Skills/8%20Handout.pdf [Last accessed on September 6, 2014]
[14].Schyve PM. Language Differences as a Barrier to Quality and Safety in Health Care: The Joint Commission Perspective. J Gen Intern Med. Nov 2007; 22(Suppl 2): 360–361.[pubmed]
[15].Dogan H, Tschudin V, Hot I. Patients’ Transcultural needs and carers’ ethical responses, Nursing Ethics 2009; 6(6): 683-696 [pubmed]
[16].Mehrabian, A. Non-verbal communication, Aldine Transaction, London 2007
[17].Canado MLP, Garcia MCG. Intercultural communication in the global workplace: The case of multicultural teams in Spain. Culture, Language and Representation, 2007; 4:185-202.
[18].Bernard A, Whitaker M, Ray M. et al., (). Impact of language barrier on acute care medical professional is dependent upon role. Journal of Professional Nursing, 2006; 22(6): 355-358[pubmed]
[19].Leavitt R.L. Competence in a Multicultural World, PT Magazine (January edition) 2003: pg 57-68
[20].Wilson C, Jones B, Lipp A. Exchanging information: patients' views on health care. Nurs Manag (Harrow). 2009 Jun;16(3):30-4.[pubmed]

