Case Report

Epiphrenic Esophageal Diverticulum: Report of a Case and Review of Literature
*Ketan Vagholkar **Rahul Kumar Chavan
- **Department of Surgery, D. Y. Patil University School of Medicine, Navi Mumbai-400706, Maharashtra, India
- Submitted February 19, 2015
- Accepted: March 24, 2015
- Published: March 24, 2015
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
Epiphrenic esophageal diverticulum is a rare entity of the esophagus. The symptoms closely mimic those of cardiac disease. Endoscopy, barium study and mannometric evaluation are necessary for a complete diagnosis.
Case Report
A case of an epiphrenic diverticulum diagnosed and treated conservatively is presented. The symptoms, diagnostic work up and therapeutic options are discussed.
Conclusions
All patients diagnosed as having an epiphrenic esophageal diverticulum should undergo a trial of conservative treatment. If the response is poor then laparoscopic intervention is the treatment of choice for treating this lesion.
Key Words
Epiphrenic Esophageal Diverticulum, Diagnosis, Treatment
Introduction
Epiphrenic esophageal diverticulum is an out pouching of esophageal lumen usually situated in the distal part of esophagus. It is typically seen within 10 cm of the cardia and usually originates from the right posterior wall [1 2]. Epiphrenic esophageal diverticulum is a rare entity. The exact incidence is unknown but prevalence may vary from 0.06 to 4 % [2]. A case of epiphrenic esophageal diverticulum presenting with mild symptoms and treated conservatively is reported along with the review of literature.
Case report
A 45 year old male patient presented with symptoms of retrosternal discomfort, regurgitation and occasional chest pain. There was no specific aggravating or relieving factors. Physical examination did not reveal any abnormality. The patient’s BMI was within normal limits. A detailed cardiac work up was carried out which did not reveal any abnormality. In view of his age and persistent retrosternal discomfort barium swallow was done which revealed an epiphrenic diverticulum arising from right side of esophagus (Figure 1). Further to this endoscopy was done to rule out any malignant lesion in the diverticulum or in the vicinity of it (Figure 2). On endoscopy the distal esophagus did not show any evidence of esophagitis or a lax lower esophageal sphincter. However antral gastritis was observed. The diverticulum had a wide mouth which could easily admit the tip of the scope (Figure 3). Manometric studies did not reveal any motility disorder. Conservative treatment was commenced comprising of proton pump inhibitors in view of antral gastritis, modification of dietary habits and meticulous consumption of water after every meal. Patient was also advised to sleep with the head end of the bed elevated. After six weeks of conservative therapy, complete resolution of symptoms was observed. Patient has been under regular follow up for last 3 years without development of symptoms and without any complications.
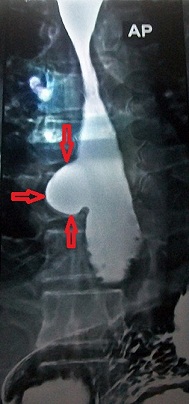
Figure 1: Barium esophagogram showing an oesophageal diverticulum marked by the red arrows

Figure 2: Endoscopic view of the diverticular opening marked by arrows

Figure 3: The endoscope negotiated across the mouth of the diverticulum
Discussion
Diverticula in the esophagus are rare [1, 2,
3]. Variation in the pressure in the lower esophagus predisposes to the development of diverticulum. Patients suffering from achalasia usually develop diverticula [4, 5]. Persistence of motility disorders lead to increase in size of diverticula. As there is an increase in size of diverticulum, there is accumulation of food particles and saliva which predispose to septic complications and eventually leading to an increase in the severity of symptoms [5]. Majority of cases closely simulate cardiac disorders leading to repeated cardiac work up [3]. Though endoscopy may help in early detection of such diverticula but in cases where the diverticulum is large and dysphagia is the presenting and predominant symptom barium swallow takes a precedence over endoscopy. The chances of malignancy in a long standing diverticulum are very high necessitating thorough endoscopic evaluation [6]. In cases where malignancy is ruled out manometric studies of the esophagus is mandatory to rule out underlying motility disorders. Majority of the diverticula are associated with motility disorders which seriously impact surgical outcomes [7, 8, 9]. Conservative treatment still holds a place of promise for treatment of epiphrenic esophageal diverticulum [6]. In mildly symptomatic patients with small sized diverticula, a trial of conservative treatment can lead to a complete remission of symptoms. So every diagnosed case of epiphrenic esophageal diverticulum should first undergo a trial of conservative treatment followed by observation of the extent of remission of symptoms. If symptoms do not resolve and persist with same severity then surgical treatment is warranted. Incidentally diagnosed cases can be treated conservatively without any compelling need for surgical intervention.
However severely symptomatic patients with a large diverticulum merit surgical intervention [10, 11]. The advent of laparoscopy has revolutionized the treatment of lower esophageal disorders. Laparoscopy has now become gold standard for treating lower esophageal disorders. Three procedures have been described for the treatment of epiphrenic esophageal diverticulum viz. diverticulectomy, esophageal seromyotomy and fundoplication [11, 12, 13].
A stapled diverticulectomy undoubtedly removes the diseased part but predisposes to staple line leakage if unaccompanied by a myotomy. Since pressure in the lower esophagus in these patients is higher than normal, a myotomy is essential to relieve the high intraluminal pressure [14, 15]. A myotomy reduces the incidence of suture line leakage as well as prevents recurrence of the diverticulum. Though the diverticulum is dealt with adequately by a combination of diverticulectomy and esophageal myotomy but the alteration in the pressure mechanics of the lower esophagus following this procedure predisposes to reflux. A fundoplication therefore needs to be incorporated in the surgical intervention. A variety of fundoplication techniques have been described [16, 17 and 18]. However, the choice of procedure depends upon whether a motility disorder is present or not. In patients without a motility disorder Nissen’s fundoplication will usually suffice, but in cases wherein a motility disorder is present Toupe’s fundoplication is preferred. Few surgeons strongly advocate an anterior Dorr partial fundoplication [19, 20, 21, 22 and 23]. The Dorr fundoplication not only prevents gastro esophageal reflux but also protects the myotomy. The advantage of Dorr fundoplication is that it is easier to perform and it prevents formation of pseudo diverticulum and leakage in the event of intra operative esophageal perforation. The risk of suture line leakage correlates with the size of the diverticulum. Diverticula more than 9 cm have higher chances of leakage, whereas use of multiple stapling shots may also predispose to suture line leakage [24, 25, 26 and 27].
Results with minimal access approach are promising (Table 1).. However availability of trained personnel is a major limiting factor in the developing world.
|
Series
|
No of patients
|
Complications (%)
|
Postoperative leakage rate (%)
|
Asymptomatic patients on follow up (%)
|
|
van der Peet et al (2001)[27]
|
5
|
20
|
20
|
-
|
|
Rosati et al (2001)[26]
|
11
|
9
|
9
|
100
|
|
Neoral et al (2002) [33]
|
3
|
33
|
33
|
-
|
|
Matthews et al (2003) [21]
|
5
|
0
|
0
|
100
|
|
Fraiji et al (2003) [30]
|
6
|
50
|
0
|
100
|
|
Klaus et al (2003) [10]
|
11
|
18
|
9
|
100
|
|
Del Genio et al (2004) [29]
|
13
|
38
|
23
|
100
|
|
Fernando et al (2005) [23]
|
20
|
45
|
20
|
83
|
|
Tedesco et al (2005) [29]
|
7
|
14
|
14
|
100
|
|
Palanivelu et al (2008) [24]
|
12
|
25
|
0
|
83
|
Conventional open surgical procedure which comprises of left thoracotomy, diverticulectomy, myotomy and Belsey Mark IV procedure has significant morbidity of up to 20- 25%. Most serious complication in this group is suture line leakage which has a mortality rate of 5% [15, 22, 27]. Other complications include thoracic pain, dysphagia, pseudo diverticulum, empyema, heart burn, pneumonia, prolonged ileus, reoperation, port site hernia and cardio vascular complications [24, 28, 29, 30,
31 amd 32]. Results of open surgery are therefore variable (Table 2).
|
Series
|
No of patients
|
Complication (%)
|
Leakage (%)
|
Asymptomatic patients on follow up (%)
|
|
Fekete et al (1992) [15]
|
27
|
19
|
10
|
78
|
|
Streitz et al (1992) [34]
|
16
|
38
|
6
|
87
|
|
Bennaci et al 1993) [18]
|
33
|
33
|
18
|
76
|
|
Altorki et al 1993) [16]
|
17
|
-
|
-
|
93
|
|
Jordan, Jr. et al., [5]
|
19
|
-
|
-
|
90
|
|
Nehra et al (2002) [35]
|
18
|
6
|
6
|
94
|
|
Varghese et al(2007) [36]
|
35
|
6
|
6
|
76
|
Though the choice of the best surgical option continues to be a subject for debate, comparison of results reveals that laparoscopic Trans hiatal resection and Heller myotomy with Dorr fundoplication is a good modality of surgical treatment for esophageal epiphrenic diverticulum as compared to open procedures [ 33, 34, 35 and36].
Conclusions
Epiphrenic esophageal diverticulum is a rare disorder of the esophagus with symptoms masquerading that of the cardiac disease.
A negative cardiac work up should warrant endoscopy for early diagnosis of epiphrenic esophageal diverticulum. Once the diagnosis is confirmed barium studies and manometry need to be done for elaborate evaluation of the magnitude of the pathological process
A symptomatic patient of epiphrenic esophageal diverticulum needs to undergo surgical intervention.
Minimally invasive approach is a promising option for these patients.
Conflict of Interests
The authors declare that there are no conflicts of interests to declare
Authors’ Contribution
KV: Literature search, preparation and editing of the manuscript.
RKC: Preparation of manuscript, table and figures literature search.
Ethical Considerations
Written informed consent was obtained from the patient for publication of this case.
Acknowledgements
We would like to thank Dr.Shirish Patil, Dean of D.Y.Patil University School of Medicine for allowing us to publish this case report.
We would also like to thank Mr. Parth Vagholkar for his help in typesetting the manuscripts.
Funding
None declared
References
[1].Herbella FA, Patti MG. Modern pathophysiology and treatment of esophageal diverticula. Langenbecks Arch Surg. 2012; 397: 29-35 [Pubmed]
[2].Orringer MB. Epiphrenic diverticula: Fact and fable. Ann Thorac Surg. 1993; 55:1067-8.[Pubmed]
[3.Cocklin JH, Singh D, Katlic MR. Epiphrenic esophageal diverticula: Spectrum of symptoms and consequences. J Am Osteopath Assoc. 2009; 109:543-5.[Pubmed]
[4].Magee Mj, Sonett JR. Management of epiphrenic esophageal diverticula. Oper Tech Thorac Cardiovasc Surg. 2011; 16:18-29
[5].Jordan PH Jr, Kinner BM. New look at epiphrenic diverticula. World J Surg. 1999; 23: 147-52 [Pubmed]
[6].Tedesco P, Fischella PM, Way LW, Patti MG. Cause and treatment of epiphrenic diverticula. Am J Surg.2005; 190: 891-4.[Pubmed]
[7].D’Journo XB, Ferraro P, Martin J, Chen LQ, Duranceau A. Lower esophageal sphincter dysfunction is part of the functional abnormality in epiphrenicdiverticulum. Br. J. Surg. 2009; 96: 892-900{pubmed]
[8].Uskudar O, Dagli U, Asil M, Yol S, Sasmaz N. Epiphrenic diverticulum with abnormal manometry: A case report. Turk J gastroenterol.2004; 15:108-11 {pubmed]
[9].Reznik SI, Rice TW, Murthy SC, Mason DP, Apperson-Hansen C, Blackstone EH. Assessment of a pathophysiology-directed treatment for symptomatic epiphrenic diverticulum. Dis Esophagus. 2007; 20: 320-7 [Pubmed]
[10].Klaus A, Hinder RA, Swain J, Achem SR. Management of epiphrenic diverticula. J Gastrointest Surg.2003; 7: 906-11 [Pubmed]
[11].Castucucci G, Porziella V, Granone PL, Picciocchi A. Tailored surgery for esophageal body diverticula. Eur J Cardiothorac Surg. 1998; 14:380-7 [Pubmed]
[12].Valentini M, Pera M, Vidal O, Lacima G, Belda J, deLacy AM. Incomplete esophageal myotomy and early recurrence of an epiphrenic diverticulum. Dis Esophagus. 2005; 18: 64-6.[Pubmed]
[13].Soares RV, Montenovo M, Pelligrini CA, Oelschlager BK. Laparoscopy as the initial approach for epiphrenic diverticula. Surg Endosc. 2011; 25: 3740-6 [Pubmed]
[14].Gonzalez-Calatayud M, Targarona EM, Balague C, Rodriguez- Luppi C, Martin AB, Trias M. Minimally invasive therapy for epiphrenic diverticula: Systematic review of literature and report of six cases. J Minim Access Surg. 2014; 10(4): 169-174.
[15].Fekete F, Vonns C. Surgical management of esophageal thoracic diverticula. Hepatogastroenterology. 1992; 39: 97-9 [Pubmed]
[16].Altorki N, Sunagawa M, Skinner DB. Thoracic esophageal diverticula: why is operation necessary? J Thorac Cardiovasc Surg. 1993; 105:260-64 [Pubmed]
[17].Olarte P, Padron OL, Arboleda D. Laparoscopic resection of an epiphrenic diverticulum. Rev Colomb Circ. 2012; 27: 306-13.
[18]1.Benacci JC, Deschamps C, Trastek VF, Allen MS, Daly RC, Pairolero PC. Epiphrenic diverticulum: results of surgical treatment. Ann Thorac Surg. 1993; 55: 1067-68[Pubmed]
[19].Plackett TP, Meghoo CA, Febinger DL. Recurrent epiphrenic diverticulum after transabdominal diverticulectomy: Report of a case and review of the literature. Image. 2009; 68: 13-5.
[20].Myers BS, Dempsey DT. Laparoscopic resection of esophageal epiphrenic diverticulum. J Laparoendosc Adv Surg Tech A. 1998; 8: 201-7.[Pubmed]
[21].Mathews BD, Nelms CD, Lohr CE, Harold KL, Kercher KW, Heniford BT. Minimally invasive management of epiphrenic esophageal diverticula. Am Surg. 2003; 69:465-70 {Pubmed]
[22].Melman L, Quinlan J, Robertson B, Brunt LM, Halpin VJ, Eagon JC, et al. Esophageal manometric characteristics and outcomes for laparoscopic esophageal diverticulectomy, myomectomy and partial fundoplication for epiphrenic diverticula. Surg Endosc. 2009; 23: 1337-41.
[23].Fernando HC, Lukettich JD, Samphire J, Alvelo Rivera M, Christie NA, Buenaventura PO, Landreneau RJ. Minimally invasive operation for esophageal diverticula. Ann thorac surg. 2005; 80: 2076-80 [Pubmed]
[24].Palanivelu C, Rangarajan M, John SJ, Parthasarthi R, Senthilkumar R. Laparoscopic transhiatal approach for benign supra-diaphragmatic lesions of the esophagus: A replacement for thoracoscopy? Dis Esophagus. 2008; 21:176-80 [Pubmed]
[25].Silecchia G, Casella G, Recchia CL, Bianchi E, Lomatire N. Laparoscopic transhiatal treatment of large epiphrenic esophageal diverticulum. JSLS. 2008.19: e 184-8.[Pubmed]
[26].Rosati R, Fumagalli U, Bona S, Zago M, Celottti S, Bisagni P. Perracchia A. Laparoscopic treatment of epiphrenic diverticula. J Laparoendosc Adv Surg Tech A. 2001; 11:371-5.[Pubmed]
[27].Van der Peet DL, Klinkenberg-Knol EC, Berends FJ, Cuesta MA. Epiphrenic diverticula: minimal invasive approach and repair in five patients. Dis Esophagus. 2001; 14:60–62[Pubmed]
[28].Kilic A, Schuchert MJ, Awais O, Luketich JD, Landreneau RJ. Surgical management of epiphrenic diverticula in the minimally invasive era. JSLS. 2009; 13:160–4 [Pubmed]
[29].Del Genio A, Rossetti G, Maffetton V, Renzi A, Brusciano L, Limongelli P, et al. Laparoscopic approach in the treatment of epiphrenic diverticula: Long-term results. Surg Endosc. 2004; 18:741–5.[[Pubmed]
[30].Fraiji E, Jr, Bloomston M, Carey L, Zervos E, Goldin S, Banasiak M, et al. Laparoscopic management of symptomatic achalasia associated with epiphrenic diverticulum. Surg Endosc. 2003; 17:1600–3.[Pubmed]
[31].Fisichella PM. Laparoscopic repair of epiphrenic diverticulum. Semin Thorac Cardiovasc Surg.2012; 24:223–8.[Pubmed]
[32].Arman Kilic, BS, Matthew J. Schuchert, MD, Omar Awais, DO, James D. Luketich, MD, and Rodney J. Landreneau, MD, Surgical Management of Epiphrenic Diverticula in the Minimally Invasive Era, JSLS. 2009 Apr-Jun; 13(2): 160–164.[Pubmed]
[33].Neoral C, Aujeský R, Bohanes T, Klein J, Král V. Laparoscopic transhiatal resection of epiphrenic diverticulum. Dis Esophagus. 2002; 15:323–325 [Pubmed]
[34].Streitz JM, Jr., Glick ME, Ellis FH., Jr Selective use of myotomy for treatment of epiphrenic diverticula. Manometric and clinical analysis. Arch Surg. 1992; 127:585–587.[Pubmed]
[35].Nehra D, Lord RV, DeMeester TR, et al. Physiologic basis for the treatment of epiphrenic diverticulum. Ann Surg. 2002; 235:346–354.[Pubned]
[36].Varghese TK, Jr., Marshall B, Chang AC, Pickens A, Lau CL, Orringer MB. Surgical treatment of epiphrenic diverticula: a 30-year experience. Ann Thorac Surg. 2007; 84:1801–1809. [Pubmed]

