Technical Innovation

Laparoscopic Treatment of Patent Omphalomesenteric Duct in Newborns Using a Linear Endoscopic Stapler
1,Yury Kozlov, 2Vladimir Novozhilov
- 1Department of Newborn surgery, Municipal Pediatric Hospital,Irkutsk State Medical Academy of Continuing Education, Irkutsk, Russia
- SubmittedThursday, February 13, 2014
- Accepted:Sunday, April 27, 2014
- PublishedFriday, June 06, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Purpose
In this work we have described our experience with repair of patent omphalomesenteric duct (POMD) by applying of stapler.
Methods
Between January 2005 and December 2012 we have performed 4 cases of the omphalomesenteric duct repaired through laparoscopy. A stapled resection was accomplished using the linear endoscopic stapler ATW35 with 2.5-mm staples (Ethicon Endo-Surgery, Cincinnati, OH). The operative report and postoperative outcomes were registered.
Results
All patients were newborns. There were 2 boys and 2 girls. The age of patients was ranged from 3 till 10 days of life. All patients were full-term and their weight of the body was ranged from 3200 to 3800 grams. The postoperative course was uneventful in the all patients. All the bowels after resection were fully functional at the end of the study.
Conclusion
The advantages of this technique are the operative time reduction and the 100% removal of an intestinal mucosa after an eversion of the Pomd.
Key words
patent omphalomesenteric duct, laparoscopy, newborn, endoscopic stapler
Introduction
A patent omphalomesenteric duct (POMD), or vitelline duct, is a form of umbilical remnant with a communication between the umbilicus and ileum that requires surgical resection. Open surgery was used long time as an effective method to treatment of POMD [1,2,3]. We report 4 cases of vitelline duct treatment with a new “double-click” laparoscopic technique. The omphalomesenteric duct was followed up to the junction with the small intestine and resected intra- and extraabdominally with usage of endoscopic articulating linear stapler.
Material and methods
Between January 2005 and December 2012 we have performed 4 cases of the omphalomesenteric duct in newborn repaired through laparoscopy with using articulated version of endoscopic linear stapler ATW35 (Ethicon Endo-Surgery, LLC Guaynabo, Puerto Rico, USA). The ethical committee of the Irkutsk Pediatric Hospital approved this study. All patients were referred to the surgeon for intermittent faecal umbilical discharge since birth. The clinical examination showed a protrusion of intestinal mucosa from the umbilicus with a central, nonvascular lumen from which the faecal discharge was produced.
Fistulography through the orifice visualized a POMD and small intestine. The surgical correction took place on next day. The standard preoperative therapy included intravenous fluid infusion and correction of the acid-base status. Preoperative antibiotic prophylaxis was administered. Laparoscopic instruments were established to the abdominal cavity through three ports
(figure 1).: two instrumental ports (first in left subcostal area - 12 mm for endoscopic stapler, second in left iliac fossa – 3 mm for endoscopic grasper) and one 5 mm optical port in right subcostal area. The omphalomesenteric duct was followed up to the junction with the small intestine, where a resection of the duct was performed by endoscopic linear stapler (first click – Figure 2). The fistula was evaginated from abdominal cavity through umbilicus using laparoscopic forceps and removed at the basis by same stapler too (second click – Figure 3).. The fascial incisions were closed using absorbable suture. Upon reaching ad libitum feeds, patients were discharged to home with a standard instruction set and 2 week, 1 month, 6 month follow-up with the operating surgeon.
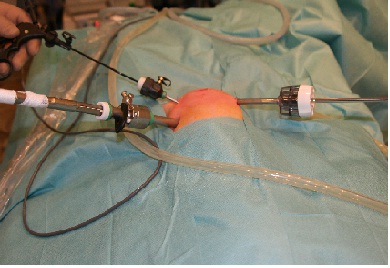
Figure 1. Position of the laparoscopic ports
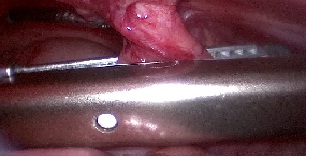
Figure 2. Creation of the first click of stapler for intra-abdominal resection of Pomd

Figure 3. Complete extraperitoneal resection of the vitelline duct (second click)
Result
All patients were newborns. There were 2 boys and 2 girls. The age of patients was ranged from 3 till 10 days of life. All patients were full-term and their weight of the body was ranged from 3200 to 3800 grams. The mean operative time was 45, 0 min (range 35-55 min). We did not compare the laparoscopic patients with patients who underwent open surgery due to the limited number of observations. The postoperative period was uneventful, and the patients were discharged from hospital on the average on postoperative day 3. A light superficial umbilical infection was observed in one patient on postoperative day 5, which resolved with regular dressings. There were found an ectopic mucosa in the two resected segment and a normal intestinal structures without ectopic tissue in two other remnants, which were confirmed by pathologic examination. The postoperative course was routine in all the patients. There were no intra- and postoperative complications. We had no intestinal leak or bleeding. We observed that the umbilical remnants and staples fell away in 5-6 days, leaving absolutely invisible scar. At follow-up bowel function was perfect in all operated patients. The infants were free from late postoperative complications such as stricture, bleeding and failure in the area of gut resection. Good intestinal transit and absorption were observed in these patients.
Discussion
Familiarity with umbilical cord anatomy is necessary to understand the abnormalities related to its remnants [4]. The omphalomesenteric duct appears very early in embryonic life as long, tubular structure that connects the midgut to the yolk sac. The vitelline duct normally regresses during the 5th - 9th week of development, leaving a solid cord that runs from the ileum to attach to the umbilicus, called the omphalomesenteric duct. If the lumen of the omphalomesenteric duct has not completely disappeared at birth, various abnormalities can result: (A) a fistula between the ileum and the umbilicus that is completely patent; (B) a sinus, with a partially patent lumen; (C) a cyst, whose intermediateportion is patent; or (D) a diverticulum, whose enteric portion is patent (ie, Meckel diverticulum). The first anomaly is very rare. It is observed in approximately 15% of the omphalomesenteric duct anomalies [5]. It usually is diagnosed during infancy. Adult presentations are extremely rare [6]. Bleeding, obstruction, and perforation are frequent complications of omphalomesenteric duct anomalies [7]. The symptomatic presentation of omphalomesenteric duct anomalies decreases with age [5]. The primary clinical characteristic of this anomaly is a feculent umbilical discharge. Although all cases of POMD are symptomatic, without intestinal prolapse or fecal discharge, the condition may be misdiagnosed as an umbilical granuloma [8].
This anomaly is treated only surgically, and treatment is recommended in all cases after diagnosis. A POMD requires surgical resection because of the possible complications such as infection of the umbilicus, bleeding from the protruded intestinal mucosa, prolapse of the intestine, strangulation ileus, and the potential for malignancy [1, 9, 10]. Usually, a laparotomy is necessary for resection of the POMD. Most resections have been performed through a transverse infraumbilical incision, a transverse supraumbilical incision, or laterally or vertically extended incision in addition to the circumumbilical approach [2, 9,10, 11]. However, these approaches produce a large, invasive operative wound.
To minimize both invasiveness and the length of the wound, a transumbilical approach was chosen via a circular incision around the mucocutaneous junction, as recommended by Shaw [12]. Wedge resection of the connection to the intestine and the umbilical plasty were performed without difficulty.
Limited reference to laparoscopic treatment of the umbilical intestinal remnant is revealed in the literature. Recently, laparoscopic techniques for diagnosis and treatment of symptomatic Meckel's diverticulum have been described [13]. At present, probably most pediatric surgeons would use laparoscopy mainly to establish the diagnosis but remove the Meckel's diverticulum in an open technique with exteriorization of the diverticulum through an enlarged umbilical incision and stapler resection [14] or use of the endoloops [15], while others would attempt to stay purely with laparoscopic technique [16,17]. We didn't find of the description of purely laparoscopic method of treatment of patent omphalomesenteric duct in newborns in literature. Although successful laparoscopic division of the omphalomesenteric ligament in two adults patients had been reported [18]. Nursal et al. [19] reported a first case of pure laparoscopic resection of symptomatic POMD in adult. We demonstrate the first newborns with detected a patent omphalomesenteric duct, which was successfully resected by laparoscopy.The role of stapling devices in surgery has continued to expand. In adults the safety and efficacy of stapled intestinal anastomosis have been extensively documented since 1978 [20]. In pediatric practice gastrointestinal staplers were applied traditionally and double-stapled anastomotic technique performing of anatomic side-by-side functioning as end-to-end anastomosis was used. Several studies have described the use of staplers in children for the treatment of Hirschsprung disease [21], appendectomy [22], and intestinal lengthening procedures [23].
There are four articles describing the use of intestinal stapler in infants for bowels join [24-28]. In 1995, Powell [24] published a series of seven newborns with a mean age of 72 days and a mean weight of 3.7 kg. Although the superiority of stapled anastomosis in newborns is not proven yet over hand-sewn anastomosis, it has definitely facilitated the ease of doing the procedure. Another benefit of stapler anastomosis is clear decrease in operative time. This may be particularly important in small, premature infants. Our previous publication [28] confirmed efficacy of the stapled anastomosis in neonates by the shorter operative time with saving equal time to full enteral feeding and length of hospital stay.
The present study further validates the use of the stapled laparoscopic resection for POMD in neonates. This technique is simple, safe, and does not require special laparoscopic skills. We did not observe complications after operations and short-term follow-up. We concluded that the age and size of patients are not the limiting factors for using of gastrointestinal staplers for resection of patent omphalomesenteric duct. The advantages of this technique are the operative time reduction and the 100% removal of an intestinal mucosa after an eversion of the POMD. The nearest future will show viability of this method.
Conclusion
Laparoscopic management of POMD with usage endoscopic articulating linear stapler is safe, effective minimally invasive surgical procedure. This report is the first to describe hybrid “double-click” laparoscopic approach for treatment of omphalomesenteric duct in newborns.
Authors' Contribution
YK: Concept, Design, preparation and editing
of the manuscript
VN: Concept, Design, preparation and editing
of the manuscript
Conflict of Interests
The authors declare that there are no conflicts of interests.
Ethical Considerations
Written informed consent was obtained for publication of these cases.
Acknowledgments
Finally, this article is addressed to former successes of Russian researchers in the field of the stapling devices which modern design was developed in the former Soviet Union [29].
Funding
None declared
References
[1].Gaisie G, Curnes JT, ScatliÄ JH, et al (1985) Neonatal intestinal obstruction from omphalomesenteric duct remnants. Am J Radiol 144:109-112 [pubmed]
[2].Miyamoto K, Furuta Y, Mukai S. (1986) Omphalomesenteric duct remnants: a review of 12 cases. J Jpn Soc Pediatr Surg 23:1048-1056
[3].Hasegawa T, Sakurai T, Monta O, et al. (1998) Transumbilical resection and umbilical plasty for patent omphalomesenteric duct. Pediatr Surg Int 13:180-181[pubmed]
[4].Sadler TW. (2012) Langman's medical embryology. Philadelphia: Wolters Kluwer Health/Lippincott Williams &Wilkins. pp 225-227
[5].Moore TC. (1996) Omphalomesenteric duct malformations. Semin Ped Surg 5:116-123 [pubmed]
[6].Ioannidis O, Paraskevas G, Kakoutis E,et al. Coexistence of multiple omphalomesenteric duct anomalies. J Coll Physicians Surg Pak 2012;22(8):524-526[pubmed]
[7].Leijonmarck CE, Bonman-Sandclin K, Frisell J, et al. (1986) Meckel's diverticulum in the adult. Br J Surg 73:146-149 [pubmed]
[8].Hinson RM, Biswas A, Mizelle KM, et al. (1997) Picture of the month: persistent omphalomesenteric duct. Arch Pediatr Adolesc Med 151:1161-1162 [pubmed]
[9].Elebute EA, Ransome-Kuti O. (1965) Patent vitello-intestinal duct with ileal prolapse. Arch Surg 91:456-460[pubmed]
[10].Van DW, West KW, Grosfeld JL. (1987) Vitelline duct anomalies. Arch Surg 122: 542-547[pubmed]
[11]Kittle CF, Jenkin HP, Dragstedt LR. (1947) Patent omphalomesenteric duct and its relation to the diverticulum of Meckel. Arch Surg 54:10-36 [pubmed]
[12].Shaw A. (1967) the umbilicus. In: Ravitch MM, Welch KJ, Benson CD, Aberdeen E, Randolph JG (eds) Pediatric surgery. Year Book Medical Publishers, Chicago, pp 771-778
[13].Lassen PM, Harris MJ, Kearse WS, et al. (1994) Laparoscopic management of incidentally noted omphalomesenteric duct remnant. J Endourol 8:49-51[pubmed]
[14].Valla JS, Steyaert H, Leculee R et al. (1998) Meckel's diverticulum and laparoscopy of children. What's new? Eur J Pediatr Surg 8:26-28 [pubmed]
[15].Schier F, Hoffmann K, Waldschmidt J. (1996) Laparoscopic removal of Meckel's diverticula in children. Eur J Pediatr Surg 6:38-39[pubmed]
[16].Teitelbaum DH, Polley TZ Jr, Obeid F. (1994) Laparoscopic diagnosis and excision of Meckel's diverticulum. J Pediatr Surg 29:495-497[pubmed]
[17].Dronov AF, Poddubnyi IV, Kotlobovskii VI et al. (2002) Videolaparoscopic surgeries in Meckel diverticulum in children. Khirururgiia 10:39-42 [pubmed]
[18].Perry CP. (1990) Recognition and treatment of persistent omphalomesenteric ligament: a report of two cases. J Reprod Med 35:636-638 [pubmed]
[19].Nursal TZ, Yildirim S, Tarim A, et al. (2002) Laparoscopic resection of patent omphalomesenteric duct in an adult. Surg Endosc. 16:1638[pubmed]
[20].Chassin J.L., Rifkind K.M., Sussman B., et al. (1978) The stapled gastrointestinal tract anastomosis: incidence of postoperative complications compared with the sutured anastomosis. Ann Surg 188:689-696
[21].Talbert J.L., Seashore J.H., Ravitch M.M. (1974) Evaluation of modified Duhamel operation for correction of Hirschsprung's disease. Ann Surg 179:671-675 [pubmed]
[22]Olguner M., Akgur F.M., Ucan B., et al. (1998) Laparoscopic appendectomy in children performed using single endoscopic GIA stapler for both mesoappendix and base of appendix. J Pediatr Surg 33:1347-1349[pubmed]
[23].Javid P.J., Kim H.B., Duggan C.P., et al. (2005) Serial transverse enteroplasty is associated with successful short-term outcomes in infants with short bowel syndrome. J Pediatr Surg 40:1019-1023[pubmed]
[24].Powell R.W. (1995) Stapled intestinal anastomosis in neonates and infants: use of the endoscopic intestinal stapler. J Pediatr Surg 30:195-197[pubmed]
[25].Wrighton L., Curtis J.L., Gollin G. (2008) Stapled intestinal anastomosis in infants. J Pediatr Surg 43:2231-2234 [pubmed]
[26].Mitchell I.C., Barber R., Fischer A.C., et al. (2011) Experience performing 64 consecutive stapled intestinal anastomosis in small children and infants. J Pediatr Surg 46:128-130[pubmed]
[27].Simmons J.D., Gunter J.W 3rd, Manley J.D., et al. (2010) Stapled intestinal anastomosis in neonates: validation of safety and efficacy. Am Surg 76:644-646[pubmed]
[28].Kozlov Y, Novogilov V, Podkamenev A, Weber I. (2013) Stapled bowel anastomoses in newborn surgery. Eur J Pediatr Surg. 23:63-66[pubmed]
[29].Astafiev GV. (1967) Investigation process relating to tissue compression in suturing and stapling apparatus. Surgical Staplers (Chirurgiceskiye Shivayushiye Apparaty), pp 22-31

