Original Article

Assessment of Training Needs of Medical Graduates in Clinical Breast Examination-Cross-Sectional Study from India
11Anita Khokhar, 2 Z. H. Khan
- 1Department of Community Medicine, Vardhman Mahavir Medical College & Safdarjung Hospital, New Delhi-110091, India
- 2Department of Physiology, North Delhi Municipal Corporation Medical College and Hindu Rao Hospital, Mallika Ganj, Tank Road, New Delhi Delhi-110007, India
- Submitted: Submitted: January 29, 2017
- Accepted: June 17, 2017
- Published: June 17, 2017
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Background
In order to be able to detect it at the earliest t is essential that the physicians are able to perform a good clinical breast exam. Also Clinical Breast Examination (CBE) presents the physician with an opportunity to make the women aware about their breasts. But whether our medical graduates are trained well enough to a good breast exam needs to be assessed.
Material and Methods
The present study was conducted in New Delhi, capital of India. Since there is paucity of literature on this topic in India the sample size was calculated with p to be 50% so as to get the maximum sample size. Allowable error was fixed at 5%. Calculated sample size was 400. Study subjects were fresh medical graduates who had completed one year of compulsory internship posting. Data was collected from students who had reported for interviews for junior residency at various hospitals both teaching as well as non-teaching located in Delhi in the year 2014. A self-administered questionnaire was prepared in English. Questionnaire was given to them to be filled after the interview was over as then subjects could be freely contacted. Data was entered in Excel sheet. Analysis was done using SPSS licensed version 21.0.Simple and cross tables were made. Also appropriate tests of significance were applied. P value of <0.05 was taken to be significant.
Results
Mean age of the participants was 23.8 years. 278(67.8%) of the participants were females and 132 (32.2%) were males. 271 (66.1%) of the participants were from a government medical college and 129 (31.5%) from private medical college. Out of a total of 410 participants 402 (98%) mentioned that they knew how to perform a CBE whereas 08 (1.95%) said they did not know how to do it. On being enquired about indications of doing a clinical breast exam majority mentioned 269 (66.9%) if a woman with a breast problem approached them then, 12 (3%) said for all women more than 40 years of age as a screening method and 121 (30.1%) mentioned in both the situations. A low proportion, 84 (20.9%) actually knew the correct perimeter of the breast. Participants also did not have adequate knowledge about the part of the hand to be used for palpation as only 116 (28.85%) responded that pads of middle three fingers should be used. Vertical strip pattern which is said to cover maximum breast area was stated by only 18 (4.5%). 99.5% (400) knew that nipples were to be examined as a part of CBE but did not know that spontaneous discharge from breast is an important sign of breast cancer. 87 (21.6%) even stated that they had never done a clinical breast exam. Only 2 (0.50%) had done more than 5 breast exams during graduation. A large number of 390 (97.0%) stated that they were not confident of doing a CBE and the main reason cited for that was not enough clinical exposure and practice. Out of 392 who stated they further wanted training main reasons cited were that as a part of general; practice this skill is required 248 (61.7%), cancer is on the increase and hence one must learn CBE, 191 (47.5%), half of the women are patients 54 (13.4%). 301/392 (74.9%) said they would like to teach the women about breast self-awareness while doing a CBE whereas 91/392 (22.6%) were apprehensive that either the lady might not understand or they might not have enough time to explain the procedure to the lady who comes to them. On being enquired about how would they like to improve their CBE skill responses were by practicing on patients 214/392 (54.6%), 174/392 (44.4%), by practicing on models/mannequin and 98(25%) by seeing videos.
Conclusion
A structured training programme for imparting skill of CBE should be formulated for the medical graduates so that they can contribute towards breast cancer screening of the large number of needy women.
Key words
Clinical breast examination, training needs assessment, India, medical graduates
Introduction
It is well evident from the data available that the survival time of women with invasive breast cancer is more if the size of the breast tumour at the time of diagnosis is small. It has also been observed that there is an inverse relationship between Clinical Breast Examination (CBE.) and the size of tumour detected by it [1]. According to Fletcher et al, physician can detect lumps as small as 3 mm by Clinical Breast Examination especially if physicians are trained on silicone breast models [2]. Although variations and inconsistencies have been there in technique of CBE all over the world but if physicians are trained in a standardized technique of doing this exam patients could benefit especially in low resource countries where quality mammography services are not freely available for screening. There has been steady increase in breast cancer cases in India and the figure is likely to go up in future and also breast cancer affects the women earlier than it does women in the west so there is a need to look at a screening modality other than mammography which may not be as effective in the younger population. A simulation study of breast cancer in India estimated that the cost of one mammogram is 3.34 times higher than that of one CBE. Also Annual CBE achieves nearly same number of life-years saved as biennial mammography, at half the cost [3]. There is a wide gap in demand for oncology services and supply in India. There is a shortage of specialists in the field of oncology as well as infrastructure for providing diagnosis s and treatment. In such a scenario, if all the physicians are trained in the skill of CBE, it may be used as a screening modality for the large population. A trial of CBE in Trivandrum has already shown down staging of the tumor in the group that was offered CBE [4]. Also CBE presents the physician with an opportunity to make the women aware about their breasts. How well are we prepared to address this issue remains to be seen as Medical Council of India has non-specific guidelines for posting in oncology and majority of medical colleges have no mandatory oncology posting [5]. Against this background, the present study was conducted to find out the training needs of the medical graduates with respect to Clinical Breast Examination.
Material and Methods
The present study was conducted in New Delhi, capital of India. Since there is paucity of literature on this topic in India the sample size was calculated with p to be 50% so as to get the maximum sample size. Allowable error was fixed at 5%.Calculated sample size was 400. Study subjects were fresh medical graduates who had completed one year of compulsory internship posting. Although Delhi has over 6 medical colleges there are large number of fresh graduates who come to Delhi every year to do junior residency in order to widen their exposure to various fields. Data was collected from students who had reported for interviews for junior residency at various hospitals both teaching as well as non-teaching located in Delhi in the year 2014. Subjects both from within Delhi and other states were included for the purpose of this study. A self-administered questionnaire was prepared in English. Questionnaire was given to them to be filled after the interview was over as then subjects could be freely contacted. They were approached till the desired sample size was achieved. All those who had done a junior residency already for 6 months their Performa was not included in the data analysis in order to have a comparable baseline. Data was entered in Excel sheet. Analysis was done using SPSS licensed version 21.0. Simple and cross tables were made. Also appropriate tests of significance were applied. p value of <0.05 was taken to be significant.
Results
Out of a total of 410 participants 402 (98%) mentioned that they knew how to perform a Clinical breast exam whereas 08 (1.95%) said they did not know how to do it. Mean age of the participants was 23.8years. 278 (67.8%) of the participants were females and 132 (32.2%) were males. 147 (35.8%) of them had graduated from Delhi and rest from other parts of the country. 271 (66.1%) of the participants were from a government medical college and 129 (31.5%) from private medical college. Most of the participants (389, 96.8%) were aware that a detailed history of existing breast problem should be taken before doing a clinical breast examination followed by 236 (58.7%) who mentioned that history of breast cancer should be enquired. Least number of 7 (1.7%) participants stated that history of mammography, ultrasound and FNAC should be asked (Table 1). 322 (80.1%) correctly knew that lump nodes should be examined in sitting position.128 (31.8%) correctly responded that axillary, supraclavicular as well as infraclavicular lymph nodes should be examined. Only 28 (7%) of the participants correctly knew that the best posture for visual inspection of breasts would ‘standing’. Only 165 (45%) correctly responded to the question regarding posture of the patient while doing a visual inspection. 154(38.3%) knew correct posture for doing palpation of the breast. Only 84 (20.9%) knew the correct perimeter of breast for the purpose of examination.116 (28.25%) of the participants correctly responded that pads of the middle three fingers should be used for a good CBE. A type of pressure to be applied to breast during a CBE was known to a dismal figure of 07 (1.7%). Vertical pattern of palpation of the breast which covers the whole breast effectively was again known to very few participants (18, 4.5%). Whether nipple should be examined while doing a CBE was correctly responded to by almost all 400 (99.5%) (Table 2). Almost half (198, 49.5%) of the participants correctly knew that CBE should be performed on a lady once a year after 40 years of age (Table 3). 87 (21.6%) even stated that they had never done a clinical breast exam. Only 2 (0.50%) had done more than 5 breast exams during graduation. 304 (75.6%) did not know the amount of time required to be spent for CBE of an average breast. 71 (17.7%) answered that 2 minutes were required to examine a breast whereas 27(6.7%) stated it to be 5 minutes. A large number of 390 (97.0%) stated that they were not confident of doing a CBE and the main reason cited for that was not enough clinical exposure and practice. They have also expressed high level desire to get training in order to improve their CBE skill. Out of 392 who stated they further wanted training main reasons cited were that as a part of general; practice this skill is required 248 (61.7%), cancer is on the increase and hence one must learn CBE 191 (47.5%), half of the women are patients 54 (13.4%) (Figure 1). 301/392 (74.9%) said they would like to teach the women about breast self-awareness while doing a CBE whereas 91/392 (22.6%) were apprehensive that either the lady might not understand or they might not have enough time to explain the procedure to the lady who comes to them. On being enquired about how would they like to improve their CBE skill responses were by practicing on patients 214/392 (54.6%), 174/392 (44.4%), by practicing on models/mannequin and 98(25%) by seeing videos. There was no statistically significant difference between the knowledge of students from government college as compared to private colleges and also between females and males p>0.05.
| |
n |
percentage |
| Breastproblemin detail |
389 |
96.8 |
| Family history of breast cancer |
236 |
58.7 |
| Hormone replacement therapy |
112 |
27.9 |
| Any breast change noticed in the past |
84 |
20.9 |
| History of breast feeding |
69 |
17.2 |
| History of alcohol, smoking, exercise |
24 |
06 |
| History of breast surgery |
12 |
03 |
| Mammography/Ultrasound/FNAC |
07 |
1.7 |
| |
number |
percentage |
| Position in which lymph node should be examined |
|
|
| Sitting |
322 |
80.1 |
| Lying down |
03 |
0.7 |
| Not sure |
18 |
2.5 |
| Group of lymph nodes to be examined |
|
|
| Axillary |
254 |
63.2 |
| Supraclavicular |
06 |
1.5 |
| Infra clavicular |
00 |
00 |
| All of the above |
128 |
31.8 |
| Not sure |
14 |
3.5 |
| Posture of the patient for visual Inspection |
|
|
| Sitting |
300 |
74.6 |
| Standing |
28 |
07 |
| Lying down |
04 |
01 |
| All of the above |
54 |
13.4 |
| Not sure |
16 |
04 |
| Position of the patient for visual inspection |
|
|
| Front and side of both the breasts |
148 |
36.8 |
| Arms overhead |
0 |
0 |
| Arms on the waist applying pressure |
68 |
16.9 |
| Leaning forwards bending at the waist |
0 |
0 |
| All of the above |
165 |
41 |
| Not sure |
21 |
5.2 |
| Posture of the patient for doing palpation |
|
|
| Lying down straight |
178 |
44.3 |
| Lying down with pillow under shoulder and arm extended at right
angle |
154 |
38.3 |
| Sitting |
70 |
17.4 |
| Knowledge about breast perimeter to be examined |
|
|
| Correct |
84 |
20.9 |
| Incorrect |
146 |
36.3 |
| Partly correct |
154 |
38.3 |
| Don’t know |
18 |
4.5 |
| Knowledge about the part of the hand with which CBE should be done |
|
|
| Flat portion of palm |
118 |
29.35 |
| Pads of middle three fingers |
116 |
28.85 |
| All fingers |
43 |
10.7 |
| Not sure |
36 |
8.95 |
| Types of pressures to be applied while doing palpation |
|
|
| One |
295 |
73.4 |
| Two |
53 |
13.2 |
| Three |
07 |
1.7 |
| Not sure |
47 |
11.7 |
| Pattern of examination of breast |
|
|
| Circular |
246 |
61.2 |
| Spoke |
24 |
6 |
| Vertical strip |
18 |
4.5 |
| Not sure |
114 |
28.35 |
| Nipple examination |
|
|
| Yes |
400 |
99.5 |
| No |
02 |
0.5 |
| |
n |
percentage |
| Once in a year after 40 years of age |
198 |
49.25 |
| Once in six months |
107 |
26.6 |
| Whenever a lady comes with breast problem |
67 |
16.7 |
| Did not know |
30 |
7.46 |

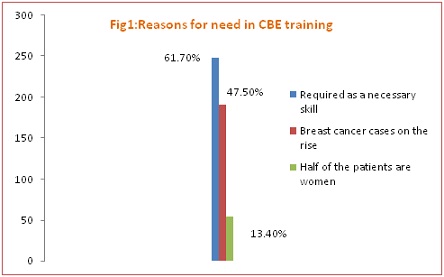
Figure 1:Reasons for need in CBE training
Discussion
In the present study, at the outset, 98% stated they knew how to perform a Clinical breast exam. In another study done among interns in Ireland 61% said they had either observed or had theoretical knowledge about breast exam and only 39% had performed it [6].
In the present study only 12 (3%) participants stated that CBE was required to be done for all women more than 40 years of age as a screening method. This shows that the participants are not yet sensitized enough towards the screening needs of women. Majority of 322 (80.1%) responded correctly that they would examine the lymph nodes in sitting position. Knowledge of group of lymph nodes to be examined was poor at 128 (31.8%). 300 (74.6%) correctly responded that the correct position to examine lymph nodes would be in sitting position. In a study by 27% of the first and second year postgraduate’s year students in surgery failed to perform axillary examination, 46% failed to perform supraclavicular region, and 36% failed to perform a visual inspection [7]. 41 (16.5%) knew of all the four positions of visual inspection of the breast. 148(36.8%) thought only inspection from front and sides was required. Only 154 (38.3%) knew about correct posture of doing palpation of the breasts. A low proportion, 84 (20.9%) actually knew the correct perimeter of the breast. Participants also did not have adequate knowledge about the part of the hand to be used for palpation as only 116 (28.85%) responded that pads of middle three fingers should be used. Several articles either advise using flat of the fingers for palpation or do not indicate what part of the finger to use [8, 9, 10]. This may also be the contributing factors towards non standardization of CBE. 07(1.7%) correctly knew that three types of pressures should be applied at a spot to properly examine the breast. Circular pattern of examination of breast was mentioned by most 246 (61.2%). According to Centre for Disease Control and the American Cancer Society best method of performing CBE is the vertical strip, three pressure methods [11,12]. Vertical strip pattern which is said to cover maximum breast area was stated by only 18 (4.5%). 400 (99.5%) knew that nipples were to be examined as a part of CBE but did not know that spontaneous discharge from breast is an important sign of breast cancer. 87 (21.6%) even stated that they had never done a clinical breast exam. Only 2 (0.50%) had done more than 5 breast exams during graduation. According to study done in Kolkota 53% of the respondents had seen less than 5 patients during their undergraduate days of cancer and about three quarter less than ten patients [13]. 304 (75.6%) did not know the amount of time required to be spent for CBE of an average breast.71 (17.7%) answered that 2 minutes were required to examine a breast whereas 27 (6.7%) stated it to be 5 minutes. According to largest increase in proportion of residents finding the breast masses occurred among those who took more than 150 seconds in which 90% of the residents found the mass [14]. Calculation of time to be taken for CBE by vertical strip pattern time required to examine both the breasts of an average patient would range from 6 to 8 minutes [15]. A large number of 390 (97.0%) stated that they were not confident of doing a CBE and the main reason cited for that was not enough clinical exposure and practice. Same, lack of exposure during the undergraduate medical education has also been cited as the main reason for lack of knowledge about cancers but others also [5, 16]. Medical students’ perceptions of their own need for additional training and the small number of CBEs they have performed has also been studied by others [12, 17, 18]. Similarly physicians have also reported lack of confidence in their CBE skills, 392 (97.5%) expressed the desire to get training in CBE whereas 10 (2.5%) mentioned they did not require further training as they were likely to take up certain other specialty in future where this would not be required [19]. They have also expressed high level desire to get training in order to improve their CBE skill. Out of 392 who stated they further wanted training main reasons cited were that as a part of general; practice this skill is required 248 (61.7%), cancer is on the increase and hence one must learn CBE, 191 (47.5%), half of the women are patients 54 (13.4%). 301/392 (74.9%) said they would like to teach the women about breast self-awareness while doing a CBE whereas 91/392 (22.6%) were apprehensive that either the lady might not understand or they might not have enough time to explain the procedure to the lady who comes to them. On being enquired about how would they like to improve their CBE skill responses were by practicing on patients 214/392 (54.6%); 174/392 (44.4%), by practicing on models/mannequin and 98 (25%) by seeing videos. As per Gaffan’s recent review of undergraduate medical education several methods are shown to be effective in teaching breast exam. These include silicone models for breast examination which increases the examiners sensitivity to the lumps, shadowing of a cancer patient by a medical student for a period of months, role pals where students deal with standardized patients. These responses were not mutually exclusive [20]. In another study by Barret et al., among third-year medical students (47 men and 49 women) at the University of Massachusetts Medical School the students with one extra training session with a standardized patient performed significantly better on the CBE [21]. Practice with immediate feedback is found to be more effective than lecture alone in teaching clinical breast examination by Pilgrim [22]. In another study conducted among students of medical college of Wisconsin although the students performed significantly better on the knowledge-based questions in their fourth year than they did in their first year, considerable room for improvement remained. The students reported learning the most from surgery rotations and more from standardized patients than from faculty. Also in their study women medical students performed significantly more clinical breast examinations than did men students. Most of the medical students reported needing additional training in clinical breast examination [23].
Conclusion
A structured training programme for imparting skill of CBE should be formulated for the medical graduates so that they can contribute towards breast cancer screening of the large number of needy women. Also it is important to directly measure their examination skills as perception of a student’s regarding their skill may not actually correspond with the required level of performance.
Acknowledgement
Heartfelt thanks to all the participants for participating in this study.
Authors Contribution
AK: Concept and design, editing of manuscriptZHK: collection of data, analysis of data and preparation of manuscript.
Ethical Consideration
The study was approved by the Institute Review Board and consent was obtained from all participants
Funding
None declared.
References
[1] Smith R A, Saslow D, Sawyer KA, Burke W, Costanza ME, Evans WP et al. American Cancer Society Guidelines for Breast Cancer Screening: Update 2003 CA. Cancer J Clin. 2003; 53: 141–169. [PubMed]
[Free
Full text]
[2] Fletcher S.W, O'Malley MS, Pilgrim CA, Gonzalez JJ. How do women compare with internal medicine residents in breast lump detection? . J Gen Intern Med. 1989; 4:277–283.[PubMed]
[3] Okonkwo QL, Draisma G, der Kinderen A, Brown ML, de Koning HJ. Breast cancer screening policies in developing countries: a cost-effectiveness analysis for India. J Natl Cancer Inst. 2008; 100: 1290–300. [PubMed]
[4] Sankaranarayanan R, Ramadas K, Thara S, Muwonge R, Prabhakar J, Augustine P et al .Clinical breast examination: preliminary results from a cluster randomized controlled trial in India. J Natl Cancer Inst .2011; 103: 1476–80. [PubMed]
[5] Sharma DN, Rath GK, Parashar A, Singh P. Survey of undergraduate medical students on their understanding and attitude towards the discipline of radiotherapy. J Cancer Res Ther. 2010; 6: 11–4. [PubMed]
[Free
Full text]
[6] Byrne D, O'Connor P, Lydon S, Kerin MJ. Preparing New Doctors for Clinical Practice: An Evaluation ofPre-Internship Training'. Irish Medical Journal 2012 105 (10):328-330. [PubMed]
[7] Chalabian, J, Garman K, Wallace P, Dunnington G. Clinical breast evaluation skills of house officers and students. Am Surg. 1996; 62: 840–84. [PubMed]
[8] Goodson WH III. Clinical breast examination. West J Med .1996; 164:355-358. [PubMed]
[PMC Full text]
[9] Henderson MA, Cawson JM, Bilous M .Breast cancer: getting the diagnosis right. Med J Austral.1995; 163:494–499. [PubMed]
[10] Isaacs JH. Physician breast examination and breast self-examination. Clin Obstet Gynecol. 1989; 32: 761–767. [PubMed]
[11] Saslow D, Hannan, J, Osuch, J. et al, Clinical breast examination: practical recommendations for optimizing performance and reporting. CA Cancer J Clin. 2004;54: 327–344. [PubMed]
[Free
Full Text]
[12] McDonald S, Saslow D, Alciati M . Performance and reporting of clinical breast examination: a review of the literature. CA Cancer J Clin.2004; 54: 345–61. [PubMed]
[Free
Full text]
[13]. Bandyopadhyay A, Das A, Ghosh A, Giri R, Biswas N. Oncology knowledge gap among freshly passed interns in a Government Medical College of Eastern India. South Asian Journal of Cancer. 2013;2:62-65. [PubMed]
[PMC Full Text]
[14]. Steiner E, Austin DF, Prouser NC. Detection and description of small breast masses by residents trained using a standardized clinical breast exam curriculum. J Gen Intern Med. 2008; 23: 129–34. [PubMed]
[PMC Full text]
[15] Pennypacker HS, Naylor L, Sander AA, Goldstein MK. Why can't we do better breast examinations?. Nurs Pract Forum. 1999; 10: 122–128. [PubMed]
[16] Wong F, Fairey RN. Radiation oncology: The misunderstood specialty. J Can Assoc Radiol. 1984; 35:144–8. [PubMed]
[17] Chalabian, J., Dunnington G. Do our current assessments assure competency in clinical breast evaluation skills? Am J Surg. 1998;175: 497–502. [PubMed]
[18] Hall DC , Adams CK, Stein, GH , Stephenson HS, Goldstein MK and Pennypacker HS Improved detection of human breast lesions following experimental training. Cancer. 1980; 46: 408–414. [PubMed]
[Free
Full text]
[19] Warner SL, Worden JK, Solomon LJ, Wadland WC. Physician interest in breast cancer screening education. A survey of Vermont family physicians. J Fam Pract 1989; 29:281-5.
[PubMed]
[20] Gaffan J, Dacre J, Jones A. Educating undergraduate medical students about oncology: a literature review. J Clin Oncol. 2006; 24: 1932–1939.
[PubMed]
[21] Barrett SV, Zapka JG, Mazor KM, Luckmann RS. Assessing third-year medical students' breast cancer screening skills. Acad Med. 2002; 77(9):905-10. [PubMed]
[22] Pilgrim C, Lannon C, Harris RP , Cogburn W, Fletcher SW Improving clinical breast examination training in a medical school J Gen Intern Med (1993) 8: 685. [PubMed]
[23] Kann PE, Lane DS. Breast cancer screening knowledge and skills of students upon entering and exiting a medical school. Acad Med. 1998 Aug; 73(8):904-6. [PubMed]

