Original Article

Knowledge, Attitudes and Perceptions of Head and Neck Radiotherapy in Ghana
*Kofi Adesi Kyei, *Reuben Vormawor, *Samuel
Yaw Opoku, *VernaVanderpuye,
- *Department of Radiography, College of Health
Sciences, Greater Accra, Accra, Ghana
- Submitted: October 22, 2014
- Accepted: January 18, 2015
- Published: January 18, 2015
Abstract
Background
Throughout the course of therapy, including radiotherapy, surgery and chemotherapy, side effects and complications can arise and have the potential to be severe and sometimes fatal. Due to the anatomic location of the vital organs of speech, swallowing and respiration, the side effects and complications of the treatment of head and neck cancers are more common than similar treatment for cancers at other anatomic sites. It is therefore important that patients’ perception about these side effects and complications of radiotherapy be established to enable the cancer management team to help patients better understand these conditions as well as the management strategies available.
Aim
The aim of the study was to investigate the knowledge, attitudes and the perceptions of patients on the side effects of head and neck radiotherapy.
Methodology
A descriptive survey with structured questionnaire as data collection tool was used. The data collected was analysed with Microsoft Excel Software and SPSS version 18. The results were presented on tables, bar charts and pie chart as well using regression analyses.
Results
The results obtained suggested that 60% of the participants had positive perception about the side effects and complications of radiotherapy, since most of them agreed that these conditions were as a result of the radiation therapy, even though, some still saw it as progression of their disease condition.
Conclusion
Head and neck cancer patients have positive perception about the side effects and complications of radiotherapy as a result of the treatment.
Key words
Perception, Side effects, Complications, Head and Neck cancers, Radiotherapy.
Introduction
Head and neck cancers are malignant tumors which affect any part of the head and neck as well as airways and digestive passages [1]. According to Jham
et al., [1] every year, about 870,000 new cases of malignant tumors on the upper airways and digestive passages are diagnosed in the world. Perception is an attitude or understanding based on what is observed, experienced or about the way one thinks about something, where as a positive attitude is a predisposition or a tendency to respond positively towards a situation of an idea. However, knowledge is the information and the understanding one has about a subject which one has in mind [2].
Patients with head and neck cancers have complex long-lasting physical and psychosocial needs due to complications associated with radiotherapy and surgeries. Studies have shown deficiencies concerning support in these respects [2 3]. The assessment of perception of side effects and complications among head and neck cancer patients has become an increasingly interesting area [4].
The term “side effect” as defined by Stedman’s Electronic Medical Dictionary, refers to a result of a drug or other therapy in addition to or in extension of the desired therapeutic effect, usually but not necessarily, connoting an undesirable effect. Complication on the other hand, is a morbid process or event occurring during a disease that is not an essential part of the disease, although it may result from it or an independent cause.
Side effects and complications of radiotherapy have been categorised into the acute tissue reactions and chronic or late tissue reactions [5]. Acute tissue reactions typically occur during treatment or shortly thereafter and they are related to the acute toxicity of the treatment from the radiation therapy. They generally resolve shortly after the termination of the therapy, but they are significant in that, they affect the patient’s quality of life during the therapy and they can become severe enough to interfere with the treatment.
The late tissue reactions are defined in the literature as occurring more than 90 days after treatment. These are more often permanent and frequently irreversible complications, they tend to be more severe. It is estimated that between 5% and 15% of head and neck cancer patients undergoing radiotherapy will have late tissue complications [6].
According to Trotti et al., [5], a systematic review of patients undergoing radiation therapy and or chemotherapy shows that, 80% of them developed severe side effects and complications such as; dysphagia, dental caries, loss of vision, hearing, taste, cataract and acute mucositis. Of these patients, one- third required hospitalization to manage these side effects and complications. In addition, 11% of the patients who were reviewed actually required an alteration or a halt in their treatment due to their mucositis [5].
It is difficult to describe the actual incidence of head and neck cancers in Ghana due to the slow rate of formation of cancer registry. Records from one of the National Centres for Cancer Management in Ghana show that in 2006, the number of head and neck cancer cases was18% (135/737) out of the total cancer cases seen in the whole year. This figure dropped to 14% in 2007 where as in 2008, 2009 and 2010, the number stood at 15 % (Ghana Cancer Registry). The incidence appears to be more prevalent among men than women and also more among the elderly than the youth [7]. The aim of the study was to establish complications of side effect of Radiotherapy at the Study site and the objectives were to
1. To evaluate patients’ perception about side effects and complications of radiotherapy.
2. To assess patients’ understanding of side effects and complication and their management.
Methodology
The research design was based on a descriptive survey using the convenience sampling method. Head and Neck cancer patients between the ages of 15 and 75 years who were in their first and second weeks of treatment were the target group. Head and neck cancers selected for the study included Nasopharyngeal (n=47), Laryngeal (n=24), Hypopharyngeal (n=10), Maxillary Antrum (n=6), Tongue (n=9) and Pituitary Adenocarcinomas (n=4). Side effects that were queried were sore throat, painful swallow, sore and dry mouth, loss of appetite as well as sleepless night, which were common with the first few weeks of treatment.
Convenient sampling method was used to obtain a sample size of 100 patients. Patients below the age 15 years and above the age of 75 years were excluded.The data collection tool used for the survey was a questionnaire. This questionnaire was a modified version of QLQ-H&N35 questionnaires for the head and neck and much focus was on the knowledge, attitudes as well as the perceptions of patients on the side effects against the objective treatment complications. It consisted four main sections, the first section; (A) was designed to obtain the demographic data from the respondents which included information on age, gender, marital status, educational background and occupation. The second section; (B) focused on the attitude of the respondents before diagnosis and during radiotherapy treatment.
The third section (C), focused on the respondents’ knowledge about head and neck cancers. The fourth section (D), focused on the respondents’ perception of side effects and complication of radiotherapy and their satisfaction about the explanations on these conditions as well as the knowledge about their management.
Patients were approached in their first and second weeks of treatment between May and July, 2013 and the times were different from patient to patient since they all had their appointment time and did not start the same day. A total of 56 out of the 100 number of the patients were undergoing concurrent chemo-radiation while 36% of the remaining 44 patients (n=16) were undergoing palliative radiotherapy. 64% (n=28) of the 44 patients were however undergoing curative radiotherapy only. All the patients received their doses prescribed by the Radiation Oncologist with a two- dimensional Cobalt teletherapy Unit technique and therefore the side effect were very much expressed. All the patients received their doses as per the case presented. All curative cases received 70Gy in 35 fractions of 2Gy daily fractions over seven weeks (44Gy for phase one, boost off-cord dose to 70Gy and post neck to 70Gy. Palliative cases were hypo-fractionated receiving 20Gy in daily fractions of 4Gy for a total of 5 days.
After signing the consent form attached to the questionnaires, the questions were read out to the patients and their responses were noted as requested by majority of the patients (81%). The rest (19%), who were mostly public servants, preferred reading the script and answering the questions by themselves. Though there was a risk of bias, authors were much focused and depending on the language chosen, questions were explained to participants before their response were noted. The data collected was organised and entered into a database and analysed using Microsoft Excel Software and SPSS version 18. The data was presented on charts, tables and regression analyses using the same software.
Approval for the study was obtained from the research ethics committee of a higher education institution. The ethics approval was supported by written permission for the study to be conducted at the study site. All study participants gave informed consent prior to the commencement of the study.
Results
All the 100 respondents recruited for the study were within the ages of 15 and 75 with the mean age of 45 years. Most of the respondents fell within the age group of 36-45 years representing 30% of the total population. The least number of respondents was however recorded within the age range of 26-35 years representing 5% of the total population. The male participants constituted 60% of the study population, while the female participants accounted for 40%. 55% of the respondents were married of which 73% were married men. The remaining 45% were either divorced, or singles
Most of the respondents fell within middle school/JSS level representing 35%. This is followed closely by 30% of the respondents with SSS level. Respondents with tertiary level formed the least with 15%. The respondents who had no formal education formed 20% of the total population. Most of the patients had no information about the disease.80% of the respondents had one form of occupation or the other and included in these were 30% farmers, 15% self-employed, 15% traders and 20% public servants. The unemployed accounted for 5% only (Table 1). 70% of the respondents were non-smokers before being diagnosed with head and neck cancer. Of the 70% non-smokers, 57% were females (Table 2).
|
Gender
|
Self-employed
|
Public
Serv.
|
Trader
|
Farmer
|
Un
employed
|
Other
|
|
Male
|
15
|
20
|
0
|
10
|
5
|
10
|
|
Female
|
0
|
0
|
15
|
20
|
0
|
5
|
|
Total(%)
|
15
|
20
|
15
|
30
|
5
|
15
|
|
Smoking
|
|
Gender
|
Yes
|
No
|
|
Male
|
30
|
30
|
|
Female
|
0
|
40
|
|
Total
|
30
|
70
|
In all it was identified that 65% of the respondents had never taken alcohol before their diagnosis (Table 3). Out of these 65%, 54% were males. Half of the respondents was informed about the side effects and complications of radiotherapy before the onset of their treatment (Table 4). In all, 60% of clients were satisfied with the explanation given them, whereas 40% were not (Table 5). In the regression analyses, the mean square of the severity of complication, knowledge and perception of patients was 2.921
(Table 6).
|
Gender
|
Yes
|
No
|
|
Male
|
25
|
35
|
|
Female
|
10
|
30
|
|
Total
|
35
|
65
|
|
Gender
|
Yes
|
No
|
|
Male
|
35
|
25
|
|
Female
|
15
|
25
|
|
Total (%)
|
50
|
50
|
|
Gender
|
Yes
|
No
|
|
Male
|
40
|
30
|
|
Female
|
20
|
10
|
|
Total (%)
|
60
|
40
|
|
Variables Entered/Removedb
|
|
Model
|
Variables Entered
|
Variables Removed
|
Method
|
|
1
|
Severity of side effects and complications of radiotherapy,
Patients Knowledge, Patients overall perception
|
|
Enter
|
|
a. All
requested variables entered
b.
Dependent Variable: age
|
|
Model Summary
|
|
Model
|
R
|
R Square
|
Adjusted R Square
|
Std. Error of the Estimate
|
|
1
|
.205a
|
.042
|
.007
|
1.557
|
|
a.
Predictors: (Constant), Severity of side effects and complications of
radiotherapy, Patients Knowledge, Patients overall perceptiona
|
|
ANOVAb
|
|
Model
|
Sum of Squares
|
df
|
Mean Square
|
F
|
Sig.
|
|
1
|
Regression
|
8.762
|
3
|
20921
|
1.205
|
.313a
|
|
Residual
|
198.726
|
82
|
2.423
|
|
|
|
Total
|
207.488
|
85
|
|
|
|
|
a.
Predictors: (Constant), Severity of side effects and complications of
radiotherapy, Patients Knowledge, Patients overall perceptiona
b.
Dependent Variable: age
|
|
Coefficientsa
|
|
Model
|
Unstandardized Coefficients
|
Standardized Coefficients
|
T
|
Sig.
|
|
B
|
Std. Error
|
Beta
|
|
1
|
(Constant)
|
3.383
|
.831
|
|
4.073
|
.000
|
|
Severity of side effects and complications of radiotherapy
|
.257
|
.173
|
.164
|
1.486
|
.141
|
|
Patients Knowledge
|
-.260
|
.404
|
-.070
|
-.644
|
.521
|
|
Patients overall perception
|
-.377
|
.331
|
-.126
|
-1.142
|
.257
|
|
a.
Dependent Variable: age
|
Sore throat, sore skin, painful swallow and loss of appetite were most common side effects and complications experienced by patients (Figure 1). Half of the patients described the side effects and complications as very severe where as 20% described it as severe (Figure 2). Most of the patients (75%) chose to seek medical help to manage the side effects and complications (Figure 3). Only 10% resorted to self-medication. In all, 60% of the patients perceived the side effects and complications as an untoward reaction to the treatment (Figure 4).
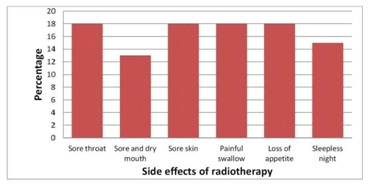
Figure 1: Common Side Effect Experienced By Respondent
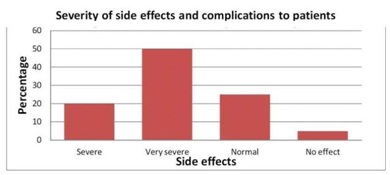
Figure 2: Severity of side effects and complications of radiotherapy
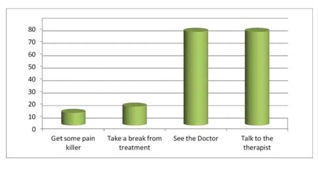
Figure 3: Patients' knowledge on the management approach to side effects of radiotherapy
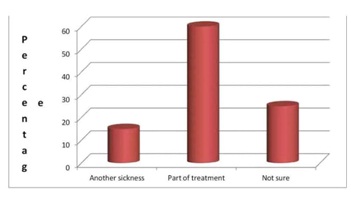
Figure 4: Patients' overall perception on the complications of radiotherapy
Discussion
The use of radiotherapy has proven to be an effective technique in the control and cure of head and neck cancers. However, the side effects and complications associated with the treatment as seen in (Figure 2) can be so severe to interfere with the treatment. In one study, for example, a five day delay in completing radiotherapy was associated with a 3.5% to 8% reduction in local control for laryngeal cancers [8]. The importance therefore, of assessing patients’ perception about the side effects and complications of radiotherapy cannot be overemphasized. It is thus required that head and neck cancer patients should be assisted to understand and demonstrate a positive attitude towards the management of side effects and complications associated with their treatment.
Demographics
The results suggested that majority of the respondents were in the age range of 36-65 years, cumulatively forming 75%. This is consistent with literature that the risk of getting cancer increases with age [9]. 75% of males showed more positive attitude and perception towards the side effects and complications of radiotherapy as compared to the 25% females. This supports literature that head and neck cancers are predominant in males than females [10]. When asked about the management approach to side effects and complications of radiotherapy, 75% of the patients chose to seek medical help when the side effects and complications occur (Figure 3). The results obtained indicated that education was one of the major factors which helped some the patients to demonstrate positive attitude and perception towards the side effects and complications of radiotherapy as well as their management. Though only 15% of them had their education to the tertiary level, those with even SSS and JSS level of education (65%) showed maturity towards the advice given them on side effects of Radiotherapy.
The economic status of the respondents (which in this study was coined to occupation) appeared to be very influencing in patients’ perception and attitude towards side effects and complications of radiotherapy ((Table 1). It was observed from the study, that patients who could afford for their treatment to be planned with CT plus dosimetry, which added additional cost to the bill of that patient experienced less side effects and complications as compared to those whose receive the conventional radiotherapy technique. In Ghana, the Radiotherapy is not under the Insurance Scheme and patient irrespective of your economic status have to pay for your bills, sometimes before the commencement of the treatment. Age was not seen as a factor in determining patients’ perception about the side effects and complications of radiotherapy, as both the young and the old participants had similar perception towards the side effects and complications (Figure 2).
As seen in the results most of the patients recruited for the study were in their first through to fourth weeks of treatment and had experienced side effects such as loss of appetite, painful swallowing, sore throat, sore and dry mouth, sore skin and sleepless night (insomnia) (Figure 1) These findings were consistent with literature on the acute tissue reactions which occur during treatment [5].
The study affirmed that age, educational level, marital status as well as Gender had a significant relationship with positive attitude towards the side effects and complications of head and neck cancers. The study also shows a significant relationship between economic status which in this case was on occupation and positive attitude.
Knowledge about Head and Neck Cancers
When the patients were asked about their knowledge about head and neck cancers
(Figure 3) it came out that, none of them about head and neck cancers before they were diagnosed of it. This was not different when the patients were asked about their main source(s) of information about the disease; all the patients claimed they had no source(s) of information on head and neck cancers. The most disturbing aspect of these results was that, well established sources of information such as; TV, radio, doctor, church, and magazines as sources for health information, education and communication were not utilised by the respondents which in the researchers opinion is very alarming
This showed that education on head and neck cancers is not reaching the target population in Ghana. With regards to radiotherapy, most of the patients got to know about it for the first time as one of the treatment modalities for head and neck cancers, when they were referred to the Hospital. There is the need therefore, to intensify education on head and neck cancers and its treatment modalities such as radiotherapy, chemotherapy and surgery.
Conclusion
Patients’ perception about side effects and complications of radiotherapy was greatly influenced by demographic factors such as gender, education, marriage, and occupation. Most of the patients had positive attitude and perception about the side effects and complications of radiotherapy as they saw these conditions as untoward effects from the treatment (Figure 4). Patients’ age however, did not significantly influence their perception about side effects and complications.
Recommendations
Based on the results of this study we recommend that;
1.There should be education on head and neck cancers in the print and electronic media, churches and schools more especially in the local languages. This will give the clients first hand information on what to do, where to go and who to see in case of any trouble.
2.The multidisciplinary cancer management team approach should be enhanced, to ensure that all who have a stake in the management of head and neck cancers are brought on board to best serve the need of the patients.
3.Simplified educational materials on the side effects and complications of radiotherapy should be made available on the bookshelves at the waiting room of every Cancer Unit for patients’ education to help them have positive attitude and perception about these conditions.
4.With increasing number of head and neck cancer patients, more oncologists and therapists should be trained and refresher courses (CPDs) on new management strategies made available for the qualified and practicing ones to improve upon their performance.
Authors’ contribution
RV and KAK, carried out the literature and prepared the draft manuscript,
SYO, and KAK carried out the experiment and VV interpreted the results,
KAK and VV designed the study and performed the analyses
SYO and RV conceived the study and participated in the study design and
KAK and VV edited the final manuscript
All authors read the script carefully and approved the final manuscript for submission
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Ethical Considerations
The authors declare that the study was approved by the Institute Ethics Committee
Funding
None declared
References
[1].Jham BC, Teixeira IV, Aboud CG, Carvalho AL, Coelho Mde M, Freire AR. A randomized phase III prospective trial of bethanechol to prevent radiotherapy-induced salivary gland damage in patients with head and neck cancer. Oral Oncol. 2007 Feb; 43(2):137-42. Epub 2006 Jun 23.
[2].Sciubba JJ, Goldenberg D. Oral complications of radiotherapy. Lancet Oncol. 2006 Feb;7(2):175-83
[Pubmed]
[3].Mittal BB, Pauloski BR, Haraf DJ, Pelzer HJ, Argiris A, Vokes EE, Rademaker A, Logemann JA. Swallowing dysfunction--preventative and rehabilitation strategies in patients with head-and-neck cancers treated with surgery, radiotherapy, and chemotherapy: a critical review. Int J RadiatOncolBiol Phys. 2003 Dec 1; 57(5):1219-30
[Pubmed]
[4].4Keefe DM, Schubert MM, Elting LS, Sonis ST, Epstein JB, Raber-Durlacher JE, Migliorati CA, McGuire DB, Hutchins RD, Peterson DE; Mucositis Study Section of the Multinational Association of Supportive Care in Cancer and the International Society for Oral Oncology. Updated clinical practice guidelines for the prevention and treatment of mucositis. Cancer. 2007 Mar 1;109(5):820-31.
[5].Trotti A, Bellm LA, Epstein JB, Frame D, Fuchs HJ, Gwede CK, Komaroff E, Nalysnyk L, Zilberberg MD. Mucositis incidence, severity and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy: a systematic literature review. RadiotherOncol. 2003 Mar; 66(3):253-62.
[Pubmed]
[6].Antonadou D1, Pepelassi M, Synodinou M, Puglisi M, Throuvalas N. Prophylactic use of amifostine to prevent radiochemotherapy-induced mucositis and xerostomia in head-and-neck cancer. Int J RadiatOncolBiol Phys. 2002 Mar 1; 52(3):739-47
[Pubmed]
[7].Robertson C, Robertson AG, Hendry JH, Roberts SA, Slevin NJ, Duncan WB, MacDougall RH, Kerr GR, O'Sullivan B, Keane TJ. Similar decreases in local tumor control are calculated for treatment protraction and for interruptions in the radiotherapy of carcinoma of the larynx in four centers. Int J RadiatOncolBiol Phys. 1998 Jan 15;40(2):319-29.
[8].Settle K, Posner MR, Schumaker LM, Tan M, Suntharalingam M, Goloubeva O, Strome SE, Haddad RI, Patel SS, Cambell EV 3rd, Sarlis N, Lorch J, Cullen KJ. Racial survival disparity in head and neck cancer results from low prevalence of human papillomavirus infection in black oropharyngeal cancer patients. Cancer Prev Res (Phila). 2009 Sep;2(9):776-81. doi: 10.1158/1940-6207.CAPR-09-0149. Epub 2009 Jul 29.
[9].Eatmon S. Cancer-an Overview. InPrinciples and Practices of Radiation Therapy,Second edition, Charles M. Washington, Dennis T. Leaver (Eds.)Mosby, 2004, 3-20
[10].Zakrzewska JM. Fortnightly review: oral cancer. BMJ. 19 99 Apr 17;318(7190):1051-4
[Pubmed]
[11].Institute of Medicine (IOM). Cancer care for the whole patient: Meeting psychosocial health needs. Nancy E. Adler and Ann E. K. Page, eds. Washington, DC: The National Academies Press. 2008 Available at http://www.ncbi.nlm.nih.gov/books/NBK4015/pdf/TOC.pdf [Last accessed on January 18, 2015]

