Original Article

Second Malignant Neoplasms in Survivors of Childhood Cancer
1,Ray M. Merrill, 2Arielle A. Sloan
- 1Department of Health Science, College of Life Sciences, Brigham Young University, Provo, Utah
- Submitted:Wednesday, March 12, 2014
- Accepted:Saturday, April 19, 2014
- PublishedThursday, May 01, 2014
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
Abstract
Introduction
Individuals who survive a first primary cancer in childhood are at increased risk of a second neoplasm.
Study design
This cohort study updates a previous report with 10 additional years of data to verify and add to our existing knowledge about subsequent cancer risk.
Materials and Methods
Analyses are based on a cohort of 40,337 children (age<20 years) who survived cancer for at least two months from 1973 through 2010 in the Surveillance, Epidemiology, and End Results (SEER) program. Each member of this cohort was followed for an average of 17.6 years. Observed/expected ratios based on cancer rates in the general population were calculated based on primary and second primary cancer types and with/without radiation treatment.
Results
Follow-up of the cohort identified 1,081 second malignant neoplasms, which represented a 4.2-fold increase in incidence compared with the general population (O/E=4.2, 95% CI=4.0-4.5). O/E ratios for subsequent cancer were consistently lower than in the first study, with the exception of Hodgkin’s lymphoma. The study also found a heightened risk of esophageal, cecum, corpus uteri, and kidney cancers among Hodgkin’s lymphoma survivors, increased risk for salivary gland tumors among CNS patients, and increased risk of the oral cavity and pharynx, respiratory system, and soft tissue second primaries among bone cancer survivors. O/E risk of subsequent neoplasm was higher among radiation-treated individuals in the current sample than in the original study
Conclusion
The increased risk and latency periods for second malignant cancer among childhood cancer patients depends on the cancer type and treatment, but risk of subsequent cancer lowers over time.
Keywords
Childhood cancer, radiotherapy, secondary neoplasms, subsequent malignancies, treatment
Background
Childhood cancer represents a major public health issue in the United States, being responsible for more child deaths from age 1 - 14 than any other cause except for motor vehicle accidents [1]. While lymphoid leukemia, lymphoma, and central nervous system (CNS) tumors account for over half of all childhood cancers, over a dozen forms of cancer manifest themselves commonly in childhood [2,5]. Regardless of type, the prevalence of childhood cancer is generally highest among males and whites [3,4] and among those who are either younger than five or between 15 and 19 years of age [5].
Advances in cancer recognition, tracking, and treatment have improved child cancer survival rates in recent years [5,6]. Since 1990, five-year survival for childhood cancers has increased in the United States from 75.1% to 83.3% and ten-year survival from 71.9% to 76.6% [5]. Now that children with cancer are surviving longer, it is important to understand their risk for subsequent malignant neoplasms later in life.
Previous research has assessed short- and long-term risks of subsequent primary cancer among survivors of childhood cancer [2,7-12]. A comprehensive body of information assembled on childhood cancer and risk of subsequent primary malignancies began in January 1970 and is called the Childhood Cancer Survivor Study [13]. The British Childhood Cancer Survivor Study identified individuals diagnosed with childhood cancer in Britain during 1940 through 1991 who had survived at least 5 years to conduct a population-based study of late mortality and the risks of second primary cancers [11].
The Surveillance, Epidemiology and End Results (SEER) Program of the National Cancer Institute has also studied new malignancies following childhood cancers diagnosed from 1973 to 2000 [2]. The current study will update the report with ten additional years of data, with the intent to verify and add to our existing knowledge about subsequent primary cancer risk. Site-specific latency periods will also be presented and results will be compared with the existing literature, which will have implications for patient follow-up monitoring.
Methods
Childhood Cancer Definition
The Childhood Cancer Survivor Study classifies childhood and adolescent cancers as those cases diagnosed before the age of 21 [13]. However, other organizations classify childhood cancers as those involving individuals younger than 20, including the SEER program of the National Cancer Institute, the Environmental Protection Agency, and the American Childhood Cancer Organization [1,10,11] In the United States, the definitive source of cancer incidence and survival data comes from the Surveillance Epidemiology and End Results (SEER) Program of the National Cancer Institute[5,6]. SEER data are currently available from 1973 through 2010 [1]. The SEER program and the International Classification for Childhood Cancer (ICCC) have provided the following list of childhood cancers: leukemia, lymphomas, CNS tumors, neuroblastoma, retinoblastoma, renal tumors, hepatic tumors, malignant bone tumors, soft tissue sarcomas, germ cell tumors, and other and unspecified malignant neoplasms [5,14,15]
SEER*Stat
SSEER*Stat is a statistical software product that provides a mechanism for SEER data analysis [16]. We used this software to compute multiple primary standardized incidence ratios, which represent the observed divided by the expected number of cancer cases subsequent to a first primary cancer diagnosis. The observed is the actual count of events resulting in the cohort. The expected number of events is what we expect to occur, based on the data in the general population and accumulated person-time at risk for this cohort. Included with the ratios are 95% confidence intervals.
We also calculated excess risk, mean age at diagnosis, and mean age when the subsequent cancer occurred. Excess absolute cancer risk is cancer incidence beyond what we normally expect. We express this as the number of excess cases of cancer per 10,000 at-risk individuals per year. Only malignant neoplasms are considered in the current study, and cases based only on death certificates or autopsies were excluded.
The data-use agreement for accessing the SEER public use data files was entered into April 24, 2013. The SEER program subsequently provided the authors with internet access to the cancer data files. We accordingly use the suggested SEER*Stat citation [16].
The SEER Program was initiated in 1973, when it began gathering and publishing population-based cancer incidence and survival data from seven tumor registries (Connecticut, Detroit [Metropolitan], Hawaii, Iowa, New Mexico, San Francisco-Oakland, and Utah). In 1975, two additional tumor registries joined the SEER Program (Seattle [Puget Sound] and Atlanta [Metropolitan]). The nine tumor registries routinely obtained cancer data in their catchment areas from the records of all cancer patients identified by hospitals, clinics, nursing homes, private pathology laboratories, radiotherapy units, death certificates, and other health service units that provide diagnostic or treatment services. The current analysis is based on SEER data collected from 1973 through 2010.
Literature Review Selection Criteria
We performed an extensive literature review to compare our results with previous research. Peer-reviewed articles published in English on second and subsequent malignant neoplasms in childhood cancer survivors during 1993-2011 were identified from electronic databases – PubMed, Wiley Online Library, Science Direct, American Association for Cancer Research, and CA: A Cancer Journal for Clinicians. The search terms used to identify all relevant published data in the above mentioned databases were: childhood cancers, second primary cancers from childhood cancer, subsequent cancers from childhood cancer, retinoblastoma, leukemia, neuroblastoma, hepatic tumor, central nervous system (CNS) tumors, lymphoma, renal tumors, malignant bone tumor, soft tissue sarcoma, germ cell tumors, thyroid tumor, skin carcinoma.
Results and Discussion
Table 1 provides description of persons
in the sample according to selected cancer sites. This study extended the study
period of the 1973-2000 original SEER report by 10 years, and, consequently,
included almost twice the number of individuals as the first study (40,337
children, as opposed to 23,819) and followed them for twice as long, on average
(17.6 years versus 8.3).
|
|
|
Number (%)
|
|
Rate per 100,000
|
Mean
|
Mean
|
Mean
|
|
Histopathology type*
|
Total
|
Male
|
Female
|
Male/Female (Ratio)
|
Age at First Primary Diagnosis
|
Age at Subsequent Primary Diagnosis
|
Latency
Period
|
|
Acute lymphocytic leukemia
|
7,578
|
4,328 (57)
|
3,250 (43)
|
3.1/2.5 (1.3)
|
7.0
|
22.1
|
15.1
|
|
Acute Myeloid
leukemia
|
1,705
|
888 (52)
|
817 (48)
|
0.6/0.6 (1.0)
|
9.5
|
25.1
|
15.6
|
|
Hodgkin lymphoma
|
3,535
|
1,821 (52)
|
1,714 (48)
|
1.3/1.3 (1.0)
|
15.8
|
34.9
|
19.1
|
|
Non-Hodgkin
lymphoma
|
2,752
|
1,863 (68)
|
889 (32)
|
1.3/0.7 (1.9)
|
12.8
|
25.9
|
13.1
|
|
Brain, CNS tumors
|
7,036
|
3,876 (55)
|
3,160 (45)
|
2.8/2.4 (1.2)
|
8.9
|
22.9
|
14.0
|
|
Neuroblastoma
|
2,154
|
1,136 (53)
|
1,018 (47)
|
0.8/0.8 (1.0)
|
2.9
|
19.9
|
17.0
|
|
Retinoblastoma
|
824
|
414 (50)
|
410 (50)
|
0.3/0.3 (1.0)
|
1.8
|
13.0
|
11.2
|
|
Renal tumors
|
1,754
|
838 (48)
|
916 (52)
|
0.6/0.7 (0.9)
|
4.5
|
21.3
|
16.8
|
|
Hepatic tumors
|
515
|
299 (58)
|
216 (42)
|
0.2/0.2 (1.0)
|
5.5
|
23.4
|
17.9
|
|
Bone tumors
|
2,277
|
1,330 (58)
|
947 (42)
|
1.0/0.7 (1.4)
|
13.8
|
27.3
|
13.5
|
|
Soft tissue sarcoma
|
3,008
|
1,621 (54)
|
1,387 (46)
|
1.2/1.0 (1.2)
|
11.0
|
24.3
|
13.3
|
|
Germ cell tumors
|
2,759
|
1,640 (59)
|
1,119 (41)
|
1.2/0.8 (1.5)
|
14.3
|
29.7
|
15.4
|
|
Thyroid carcinoma
|
1,546
|
307 (20)
|
1,239 (80)
|
0.2/0.9 (0.2)
|
16.5
|
34.6
|
18.1
|
|
Melanoma
|
1,329
|
533 (40)
|
796 (60)
|
0.4/0.6 (0.7)
|
16.3
|
26.7
|
10.4
|
|
Wilms’ tumor
|
1,565
|
741 (47)
|
824 (53)
|
0.5/0.6 (0.8)
|
3.9
|
22.1
|
18.2
|
Data source: Surveillance, Epidemiology, and End Results (SEER). Note: Includes children surviving 2 months or more after diagnosis. CNS: Central Nervous System.*Categories and ordering based on International Classification of Childhood Cancer [15].
The results of this study generally reflected findings from the 1973-2000 SEER report, such as the fact that acute lymphocytic leukemia remained the most common type of first cancer (accounting for 19% of cases, similar to the originally reported 21%), while 17% were CNS cancers (as opposed to 18% in the first study) [2]. Mean age at first cancer diagnosis also remained similar to the first study, both overall and stratified by gender [2]. The shortest latency period involved first primary melanoma, and the longest latency period involved first primary Hodgkin lymphoma. However, a number of differences were noted between this study and the original, which will be described in detail in this section.
Increased risk of being diagnosed with a subsequent cancer is
presented for several cancer sites in Figure 1. For example
children diagnosed with acute lymphocytic leukemia had a 3.7 times greater risk of being diagnosed with a subsequent cancer compared with the general population.
Children diagnosed with CNS tumors had a 5.2 times greater risk of a subsequent cancer. Children diagnosed with thyroid carcinoma were least likely to have a subsequent cancer event, whereas children diagnosed with retinoblastoma were most likely to have a subsequent cancer event. The figure also shows site-specific excess cancers (beyond the expected amount) per 10,000 persons per year. Excess cancers for acute lymphocytic leukemia were low compared with that of most of the other childhood cancers. Excess cancers for CNS was over twice that of acute lymphocytic leukemia but were lower than those for non-Hodgkin lymphoma, bone tumors, Hodgkin lymphoma, and retinoblastoma.
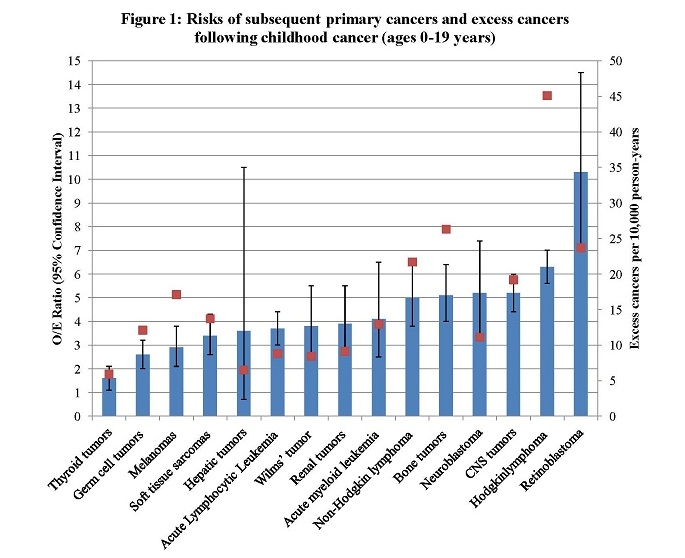
Table 2 and Table 3 show the risk of subsequent cancer based on first cancer diagnosis and use of radiation treatment. Subsequent cancer risk among childhood cancer survivors especially among patients who underwent radiation treatment was greater than
the cancer risk in the general population, as reported in the original study [2]. Still, in several cases, higher O/E ratios were not statistically significant, and in other cases, small counts influenced reported associations.
|
|
|
|
|
|
|
Age at First Primary Diagnosis
|
Latency
Period
|
Bone
|
Brain, CNS
|
Thyroid
|
Leukemia
|
|
Histopathology type*
|
No.
|
%
|
O/E
|
95% CI Lower
|
95% CI Upper
|
Mean
|
Mean
|
O/E
|
O/E
|
O/E
|
O/E
|
|
Acute lymphocytic leukemia
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
71
|
68
|
4.0
|
3.1
|
5.1
|
6.6
|
14.2
|
6.8
|
8.1
|
7.4
|
4.8
|
|
Yes
|
33
|
32
|
3.1
|
2.1
|
4.3
|
8.2
|
16.8
|
13.0
|
12.5
|
7.9
|
|
|
Acute myeloid
leukemia
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
12
|
50
|
3.2
|
1.6
|
5.6
|
9.5
|
26.8
|
|
7.4
|
|
|
|
Yes
|
12
|
50
|
10.2
|
3.8
|
22.3
|
10.0
|
12.7
|
|
26.5
|
27.6
|
|
|
Hodgkin lymphoma
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
78
|
26
|
5.0
|
3.9
|
6.2
|
15.7
|
16.7
|
10.8
|
7.7
|
9.2
|
18.1
|
|
Yes
|
217
|
74
|
6.9
|
6.1
|
7.9
|
15.8
|
20.0
|
12.9
|
|
8.0
|
7.5
|
|
Non-Hodgkin
lymphoma
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
29
|
50
|
4.3
|
2.9
|
6.2
|
12.6
|
11.5
|
|
|
8.3
|
12.1
|
|
Yes
|
29
|
50
|
5.9
|
3.9
|
8.4
|
13.1
|
14.7
|
23.6
|
|
19.4
|
8.2
|
|
Brain, CNS tumors
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
58
|
33
|
3.7
|
2.8
|
4.7
|
8.4
|
12.0
|
|
18.1
|
|
6.5
|
|
Yes
|
116
|
67
|
6.5
|
5.4
|
7.8
|
9.3
|
14.8
|
20.4
|
47.7
|
8.5
|
11.9
|
|
Neuroblastoma
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
14
|
45
|
3.5
|
1.9
|
5.8
|
2.5
|
14.0
|
|
|
|
|
|
Yes
|
17
|
55
|
8.6
|
5.0
|
13.8
|
3.8
|
18.9
|
|
|
21.8
|
|
|
Retinoblastoma
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
13
|
39
|
5.1
|
2.7
|
8.8
|
1.8
|
7.9
|
51.3
|
|
|
|
|
Yes
|
20
|
61
|
29.6
|
18.1
|
45.7
|
1.4
|
13.7
|
311.6
|
|
|
29.4
|
|
Renal tumors
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
13
|
42
|
3.3
|
1.7
|
5.6
|
4.4
|
15.4
|
|
|
|
|
|
Yes
|
18
|
58
|
4.5
|
2.7
|
7.1
|
4.7
|
17.8
|
|
|
7.1
|
|
|
Hepatic tumors
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
3
|
100
|
3.7
|
0.8
|
10.8
|
5.4
|
18
|
|
|
|
|
|
Yes
|
0
|
0
|
|
|
|
|
|
|
|
|
|
|
Bone tumors
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
48
|
67
|
4.3
|
3.1
|
5.7
|
13.9
|
14.5
|
11.7
|
|
5.0
|
19.5
|
|
Yes
|
24
|
33
|
8.4
|
5.4
|
12.5
|
13.5
|
11.7
|
102.0
|
|
|
35.5
|
|
Soft tissue sarcoma
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
22
|
33
|
1.6
|
1.0
|
2.4
|
11.4
|
12.8
|
15.1
|
6.0
|
|
|
|
Yes
|
45
|
67
|
7.3
|
5.4
|
9.8
|
10.6
|
13.7
|
48.7
|
5.2
|
|
15.3
|
|
Germ cell tumors
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
60
|
80
|
2.5
|
1.9
|
3.2
|
14.2
|
13.8
|
|
|
|
5.9
|
|
Yes
|
15
|
20
|
2.8
|
1.6
|
4.6
|
14.6
|
22.2
|
|
18.6
|
|
|
|
Thyroid carcinoma
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
26
|
67
|
1.5
|
1.0
|
2.2
|
16.5
|
19.7
|
|
|
|
|
|
Yes
|
13
|
33
|
1.8
|
1.0
|
3.1
|
16.5
|
14.9
|
|
|
|
|
|
Melanoma
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
48
|
100
|
2.9
|
2.1
|
3.8
|
16.3
|
10.4
|
|
|
|
|
|
Yes
|
0
|
0
|
|
|
|
|
|
|
|
|
|
|
Wilms’ tumor
|
|
|
|
|
|
|
|
|
|
|
|
|
No
|
10
|
37
|
3.0
|
1.5
|
5.8
|
3.3
|
16.9
|
|
|
|
|
|
Yes
|
17
|
63
|
4.4
|
2.5
|
7.0
|
4.6
|
18.7
|
|
|
7.1
|
|
|
Histopathology type*
Subsequent Cancer Site
|
Observed
|
Observed/Expected
|
95% CI Lower
|
95% CI Upper
|
Excess Cancers
Per 10,000
|
Mean Latency Period
|
Supporting References
|
|
Acute Lymphocytic Leukemia
|
|
|
|
|
|
|
|
|
Oral Cavity and Pharynx
|
9
|
16.0
|
7.3
|
30.4
|
1.0
|
15.7
|
2, 36
|
|
Salivary Gland
|
8
|
45.6
|
19.7
|
89.9
|
0.9
|
16.2
|
2, 32, 36
|
|
Bones and Joints
|
7
|
8.5
|
3.4
|
17.6
|
0.7
|
8.4
|
2, 31, 34
|
|
Soft Tissue including Heart
|
7
|
7.6
|
3
|
15.6
|
0.7
|
8.4
|
31, 37
|
|
Brain, CNS
|
24
|
9.3
|
6.0
|
13.9
|
2.5
|
14.2
|
2, 31, 33, 34, 35
|
|
Thyroid
|
21
|
7.6
|
4.7
|
11.6
|
2.1
|
20.0
|
2, 31, 33, 34
|
|
Leukemia
|
13
|
4.6
|
2.4
|
7.8
|
1.2
|
9.0
|
34
|
|
Non-Lymphocytic Leukemia
|
13
|
12.1
|
6.4
|
20.6
|
1.4
|
9.0
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
11
|
13.8
|
6.9
|
24.7
|
1.2
|
9.9
|
|
|
Myeloid and Monocytic Leukemia
|
13
|
13.2
|
7.0
|
22.6
|
1.4
|
9.0
|
|
|
Acute Myeloid Leukemia
|
11
|
16.3
|
8.1
|
29.1
|
1.2
|
9.9
|
31, 32, 38
|
|
Acute Myeloid Leukemia
|
|
|
|
|
|
|
|
|
Brain, CNS
|
3
|
9.7
|
2.0
|
28.4
|
2.5
|
17.7
|
31
|
|
Thyroid
|
3
|
6.8
|
1.4
|
19.9
|
2.4
|
17.4
|
31
|
|
Hodgkin Lymphoma
|
|
|
|
|
|
|
|
|
Salivary Gland
|
7
|
32.1
|
12.9
|
66
|
1.2
|
21.1
|
2
|
|
Esophagus
|
4
|
27.3
|
7.4
|
69.9
|
0.7
|
26.9
|
|
|
Colon excluding Rectum
|
9
|
6.3
|
2.9
|
12
|
1.4
|
29.6
|
2, 7, 27, 47, 49
|
|
Stomach
|
7
|
18.5
|
7.4
|
38.2
|
1.2
|
19.1
|
2, 7, 49
|
|
Cecum
|
3
|
13.2
|
2.7
|
38.6
|
0.5
|
30.2
|
|
|
Soft Tissue including Heart
|
19
|
23.7
|
14.3
|
37
|
3.3
|
15.7
|
2, 31, 51
|
|
Melanoma of the Skin
|
12
|
2.2
|
1.1
|
3.8
|
1.2
|
17.3
|
2, 7, 17, 43, 47, 50
|
|
Female Breast
|
96
|
11.4
|
9.2
|
13.9
|
15.9
|
20.9
|
2, 7, 8, 10, 17, 27, 31, 32, 38,
42-48
|
|
Pancreas
|
4
|
11.1
|
3
|
28.4
|
0.7
|
18.8
|
2
|
|
Lung and Bronchus
|
12
|
8.2
|
4.2
|
14.3
|
1.9
|
24.3
|
2, 49, 51
|
|
Bones and Joints
|
6
|
12.1
|
4.4
|
26.4
|
1.0
|
9.5
|
2, 7, 17, 27, 31, 49, 51
|
|
Corpus Uteri
|
4
|
3.9
|
1.1
|
10
|
0.5
|
19.4
|
|
|
Kidney
|
7
|
6.6
|
2.7
|
13.7
|
1.1
|
30.9
|
|
|
Brain, CNS
|
6
|
3.3
|
1.1
|
7.2
|
0.8
|
16.7
|
2, 7, 17, 27, 31, 49, 51
|
|
Thyroid
|
37
|
8.4
|
5.9
|
11.6
|
5.9
|
16.4
|
2, 7, 17, 27, 31, 32, 43
|
|
Non-Hodgkin Lymphoma
|
18
|
6.7
|
3.9
|
10.5
|
2.8
|
18.2
|
2, 7, 17, 27, 31, 32, 39
|
|
Leukemia
|
19
|
11.3
|
6.8
|
17.7
|
3.1
|
5.6
|
2, 7, 17, 27, 31, 48
|
|
Non-Lymphocytic Leukemia
|
18
|
17.2
|
10.2
|
27.3
|
3.1
|
5.6
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
17
|
25.1
|
14.6
|
40.2
|
3.0
|
5.5
|
2
|
|
Myeloid and Monocytic Leukemia
|
16
|
16.5
|
9.5
|
26.9
|
2.7
|
5.4
|
|
|
Acute Myeloid Leukemia
|
15
|
25.4
|
14.2
|
41.8
|
2.6
|
5.1
|
31
|
|
Non-Hodgkin Lymphoma (except Burkitt
Lymphoma)
|
|
|
|
|
|
|
Female Breast
|
7
|
5.8
|
2.3
|
12
|
2.7
|
25.3
|
2,
7, 13, 17, 31, 35, 47, 51, 58, 59
|
|
Brain
|
3
|
4.9
|
1
|
14.3
|
1.1
|
2.1
|
17, 41, 51, 58, 59
|
|
Thyroid
|
13
|
12.8
|
6.8
|
21.8
|
5.6
|
16.4
|
2, 7, 13, 17, 31, 32, 47,51, 52
|
|
Lymphoma
|
11
|
6.8
|
3.4
|
12.2
|
4.4
|
8.3
|
7, 17, 31, 53, 58, 59
|
|
Non-Hodgkin Lymphoma
|
6
|
7.3
|
2.7
|
15.8
|
2.4
|
9.4
|
31, 48, 58
|
|
Leukemia
|
7
|
10.7
|
4.3
|
22
|
3.0
|
1.7
|
2, 7, 59
|
|
Non-Lymphocytic Leukemia
|
7
|
20.0
|
8.0
|
41.2
|
3.1
|
1.7
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
6
|
25.5
|
9.4
|
55.6
|
2.7
|
0.6
|
2
|
|
Myeloid and Monocytic Leukemia
|
7
|
21.6
|
8.7
|
44.5
|
3.1
|
1.7
|
|
|
Acute Myeloid Leukemia
|
4
|
19.6
|
5.3
|
50.1
|
1.8
|
1.5
|
59
|
|
Brain, CNS tumors
|
|
|
|
|
|
|
|
|
Salivary Gland
|
4
|
21.3
|
5.8
|
54.6
|
0.5
|
17
|
|
|
Rectum and Rectosigmoid Junction
|
3
|
5.7
|
1.2
|
16.7
|
0.3
|
13.8
|
2, 47, 49, 53, 54
|
|
Liver
|
3
|
13.7
|
2.8
|
39.9
|
0.4
|
18.1
|
53
|
|
Pancreas
|
2
|
10.1
|
1.2
|
36.5
|
0.2
|
12
|
2
|
|
Bones and Joints
|
9
|
12.7
|
5.8
|
24.1
|
1.1
|
9.1
|
2, 7, 17, 31, 34, 51, 54
|
|
Soft Tissue including Heart
|
13
|
14.8
|
7.9
|
25.3
|
1.7
|
11.1
|
2, 31, 51, 53
|
|
Brain, CNS
|
72
|
32.3
|
25.3
|
40.7
|
9.5
|
15.4
|
2, 7, 13, 17, 31, 34, 40, 41, 48, 51,
52, 54
|
|
Thyroid
|
17
|
5.4
|
3.1
|
8.6
|
1.9
|
18.2
|
7, 13, 17, 31, 34, 48, 49, 51, 52, 53
|
|
Leukemia
|
21
|
9.1
|
5.6
|
13.8
|
2.6
|
4.8
|
7, 17, 31, 34, 51, 54
|
|
Lymphocytic Leukemia
|
7
|
5.5
|
2.2
|
11.3
|
0.8
|
6.5
|
|
|
Acute Lymphocytic Leukemia
|
6
|
5.1
|
1.9
|
11.1
|
0.7
|
2.9
|
2, 33
|
|
Non-Lymphocytic Leukemia
|
14
|
13.4
|
5.6
|
13.8
|
2.6
|
2.9
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
12
|
16.3
|
8.4
|
28.4
|
9.8
|
4.1
|
|
|
Myeloid and Monocytic Leukemia
|
14
|
14.6
|
8.0
|
24.4
|
1.8
|
3.9
|
|
|
Acute Myeloid Leukemia
|
12
|
18.9
|
9.8
|
33.1
|
1.6
|
4.1
|
53,
54
|
|
Neuroblastoma and Other Peripheral
Nervous Cell Tumors
|
|
|
|
|
|
|
|
|
Digestive System
|
6
|
18.9
|
6.9
|
41.2
|
2.5
|
16.9
|
2
|
|
Kidney
|
7
|
35.5
|
14.3
|
73.1
|
3.0
|
16.3
|
2, 56
|
|
Thyroid
|
4
|
8.2
|
2.2
|
21.1
|
1.6
|
16.3
|
2, 7, 13, 31, 33, 48, 49, 51, 56, 57
|
|
Retinoblastoma
|
|
|
|
|
|
|
|
|
Nose, Nasal Cavity and Middle Ear
|
3
|
325.5
|
67.1
|
951.1
|
2.4
|
11
|
49, 61, 62
|
|
Bones and Joints
|
11
|
109.5
|
54.7
|
196
|
8.7
|
9
|
2, 15, 16, 49, 51, 54
|
|
Eye and Orbit - Non-Melanoma
|
4
|
107.2
|
29.2
|
274.5
|
3.2
|
9.6
|
2
|
|
Soft Tissue including Heart
|
3
|
22.4
|
4.6
|
65.6
|
2.3
|
16.2
|
2, 49, 51, 62
|
|
Leukemia
|
4
|
8.6
|
2.4
|
22.1
|
2.8
|
9
|
|
|
Acute Lymphocytic Leukemia
|
4
|
12.8
|
3.5
|
32.8
|
2.9
|
9
|
2
|
|
Renal Tumors
|
|
|
|
|
|
|
|
|
Kidney
|
5
|
25.0
|
8.1
|
58.4
|
1.9
|
12.3
|
|
|
Soft Tissue including Heart
|
5
|
18.2
|
5.9
|
42.5
|
1.9
|
12.7
|
31
|
|
Thyroid
|
4
|
4.9
|
1.3
|
12.5
|
1.3
|
20.4
|
31, 54
|
|
Leukemia
|
4
|
4.8
|
1.3
|
12.3
|
1.1
|
7.4
|
52
|
|
Non-Lymphocytic Leukemia
|
3
|
9.8
|
2
|
28.7
|
1.1
|
6.2
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
3
|
13.2
|
2.7
|
38.5
|
1.1
|
6.2
|
|
|
Myeloid and Monocytic Leukemia
|
3
|
10.8
|
2.2
|
31.7
|
1.1
|
6.2
|
|
|
Acute Myeloid Leukemia
|
3
|
15.6
|
3.2
|
45.7
|
1.1
|
6.2
|
|
|
Bone Tumors
|
|
|
|
|
|
|
|
|
Oral Cavity and Pharynx
|
3
|
8.9
|
1.8
|
26.0
|
1.2
|
31.8
|
|
|
Colon excluding Rectum
|
3
|
7.1
|
1.5
|
20.8
|
1.2
|
19.5
|
7, 13, 52
|
|
Respiratory System
|
3
|
5.7
|
1.2
|
16.8
|
1.1
|
17.2
|
|
|
Bones and Joints
|
7
|
31.8
|
12.8
|
65.6
|
3.1
|
4.1
|
7, 34, 48, 52, 54, 60
|
|
Soft Tissue including Heart
|
8
|
27.2
|
11.7
|
53.6
|
3.5
|
10.7
|
|
|
Kidney
|
3
|
9.5
|
2
|
27.7
|
1.2
|
18.7
|
|
|
Thyroid
|
5
|
3.9
|
1.3
|
9.1
|
1.7
|
14.1
|
13, 17, 34, 51, 52, 54
|
|
Female Breast
|
14
|
6.6
|
3.6
|
11.1
|
5.4
|
19
|
7, 10, 13, 17, 31, 34, 47, 52, 60
|
|
Leukemia
|
15
|
23
|
12.9
|
37.9
|
6.5
|
4.5
|
7, 34, 48, 52, 54, 55
|
|
Non-Lymphocytic Leukemia
|
14
|
37.5
|
20.5
|
62.9
|
6.2
|
3.9
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
14
|
55.9
|
30.6
|
93.8
|
6.3
|
3.9
|
|
|
Myeloid and Monocytic Leukemia
|
14
|
40.4
|
22.1
|
67.8
|
6.2
|
3.9
|
|
|
Acute Myeloid Leukemia
|
11
|
50.2
|
25.1
|
89.9
|
4.9
|
4.9
|
|
|
Acute Monocytic Leukemia
|
3
|
178.9
|
36.9
|
522.9
|
1.4
|
0.3
|
|
|
Soft Tissue Sarcomas
|
|
|
|
|
|
|
|
|
Oral Cavity and Pharynx
|
5
|
10.7
|
3.5
|
25.1
|
1.3
|
17.7
|
2
|
|
Tongue
|
3
|
25.8
|
5.3
|
75.4
|
0.8
|
12.6
|
9, 49
|
|
Lung and Bronchus
|
3
|
5.4
|
1.1
|
15.8
|
0.7
|
22
|
9, 49
|
|
Bones and Joints
|
9
|
28
|
12.8
|
53.2
|
2.5
|
9.4
|
2, 7, 17, 31, 34, 49, 51, 52, 54
|
|
Soft Tissue including Heart
|
9
|
20.2
|
9.2
|
38.4
|
2.5
|
11.6
|
9, 31, 34, 51
|
|
Kidney
|
3
|
6.3
|
1.3
|
18.4
|
0.7
|
12.9
|
|
|
Brain, CNS
|
6
|
5.7
|
2.1
|
12.5
|
1.4
|
17.6
|
7, 13, 17, 34, 31, 41, 54
|
|
Lymphatic and Hematopoietic Diseases
|
9
|
2.5
|
1.2
|
4.8
|
1.6
|
5.7
|
|
|
Leukemia
|
8
|
7.4
|
3.2
|
14.6
|
2.0
|
6.3
|
7, 9, 17, 31, 34, 48, 49, 54
|
|
Non-Lymphocytic Leukemia
|
8
|
14.6
|
6.3
|
28.9
|
2.2
|
6.3
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
7
|
18.8
|
7.6
|
38.8
|
1.9
|
6.6
|
|
|
Myeloid and Monocytic Leukemia
|
8
|
15.9
|
6.9
|
31.3
|
2.2
|
6.6
|
|
|
Acute Myeloid Leukemia
|
7
|
21.8
|
8.7
|
44.8
|
1.9
|
6.6
|
9
|
|
Germ Cell Tumors
|
|
|
|
|
|
|
|
|
Testis
|
28
|
13.1
|
8.7
|
19
|
6.9
|
12
|
2, 52
|
|
Brain, CNS
|
6
|
4.8
|
1.8
|
10.5
|
1.3
|
5.5
|
|
|
Lymphatic and Hematopoietic Diseases
|
11
|
2.4
|
1.2
|
4.3
|
1.7
|
18.9
|
|
|
Leukemia
|
7
|
5.7
|
2.3
|
11.7
|
1.5
|
12.5
|
54
|
|
Non-Lymphocytic Leukemia
|
6
|
8.6
|
3.1
|
18.6
|
1.4
|
12.6
|
|
|
Acute Non-Lymphocytic Leukemia (ANLL)
|
5
|
10.9
|
3.5
|
25.4
|
1.2
|
11.5
|
|
|
Myeloid and Monocytic Leukemia
|
6
|
9.2
|
3.4
|
20.1
|
1.4
|
12.6
|
|
|
Acute Myeloid Leukemia
|
4
|
10
|
2.7
|
25.5
|
1.0
|
13.2
|
|
|
Thyroid Carcinomas
|
|
|
|
|
|
|
|
|
Salivary Gland
|
4
|
35.6
|
9.7
|
91.1
|
1.6
|
8.0
|
|
|
Kidney
|
3
|
6.6
|
1.4
|
19.2
|
1.1
|
25.7
|
|
|
Malignant Melanomas
|
|
|
|
|
|
|
|
|
Melanoma of the Skin
|
38
|
18.3
|
13.0
|
25.1
|
19.7
|
9.6
|
|
|
Wilms’ Tumor
|
|
|
|
|
|
|
|
|
Soft Tissue including Heart
|
5
|
19.7
|
6.4
|
45.9
|
2.0
|
13.3
|
34, 51
|
|
Thyroid
|
4
|
5.4
|
1.5
|
13.8
|
1.4
|
21.0
|
7, 13, 34, 51
|
|
|
| |
|
Data source: Surveillance, Epidemiology, and End Results (SEER).
Note: Includes children surviving 2 months or more after diagnosis. CNS: Central Nervous System.
Categories and ordering based on International Classification of Childhood Cancer [15].
In our study, there was a 4.2-fold higher subsequent cancer incidence among childhood cancer survivors compared with the general population (O/E = 4.2, 95% CI = 4.0-4.5), which is significantly lower than the 6-fold O/E ratio observed in the previous study [2]. Cancer-specific O/E ratios were generally lower for cancers in this analysis regardless of whether or not radiation treatment was used, although these differences were generally non-significant. Two exceptions included Hodgkin’s lymphoma, which had a 6.9 subsequent cancer O/E ratio if treated with radiation and 5.0 without, as opposed to 1.2 and 0.35, respectively; and non-Hodgkin’s lymphoma without radiation treatment, which had a 4.3 O/E ratio as opposed to 2.85 [2]. The general decrease in the O/E ratio would be expected not only because cancer treatments and early detection have improved but because the impact of childhood cancer on subsequent cancer risk tends to lower with age [2]. Further study should be conducted to determine whether the O/E ratio among Hodgkin’s lymphoma survivors and among non-Hodgkin’s lymphoma survivors who did not undergo radiation treatment will continue to increase.
Concerning gender disparities, the male:female ratio of first cancer cases remained 54:46, and females in our study were still overrepresented for melanoma and Wilms’ tumor [2]. However, rather than outnumbering males for fibrosarcoma and carcinoma, as was the case in the original study, females outnumbered males for renal and thyroid cancers. Mean age at diagnosis was similar between males and females (10.1 versus 10.2 for females), as found previously, but mean age at a subsequent event was lower for males than for females (25.6 vs. 28.8). Increased risk of subsequent cancer was influenced by follow-up time (O/E = 5.6 [3.8-8.0] for 2-11 months, 7.3 [6.2-8.5] for 12-59 months, 6.9 [6.0-7.9] for 60-119 months, and 3.4 [3.2-3.7] for 120+ months).The original SEER study did not include O/E ratios for esophageal and cecal cancer among Hodgkin’s disease survivors, salivary gland tumors among CNS survivors, or oral cavity, pharynx, respiratory and soft tissue cancers among bone cancer patients.In addition, no studies from our literature review identified specific links between these primary and second primary cancers.In our study, however, there was a significant association observed for each.
The fact that this study found these and other associations
among cancers for the first time may be due in part to the 10 years of follow-up
that have been added since the original SEER report. Both Hodgkin’s and bone
cancer, for example, were diagnosed at later ages in our study (15.8 years and
13.8, respectively), with latency periods of 19.1 and 13.5 years before the
subsequent primary cancer (Table 1). In the original study, patients were followed up on average for only 8.3 years [2]. Regardless, further research on each of these subjects would prove valuable, especially because the second primary cancers described above are most commonly diagnosed after middle age [68].
Several studies have emphasized the importance of long-term follow-up when investigating second malignant neoplasms[10,
18, 19, 34,
42],[49], [52] and [57]. In our study, typically 15.2 years separated the first and subsequent neoplasm. The previous SEER-based study of new malignancies following childhood cancer included 10 fewer years in its analysis and failed to observe some of the findings observed in the current study, especially among individuals who were diagnosed with cancers later in childhood. The latency periods presented in this study should guide further research on the length of follow-up needed, and continued follow-up on this population should determine how risk of subsequent cancer changes over time.
Conclusions
The current study verifies several previous studies showing that children who survive various types of cancer are at increased risk of developing certain second malignant neoplasms. With follow-up, these excess cancer rates remain higher than the general population but may either lower or increase during specific ages.
In addition to confirming several of the previously shown results, children with a first primary Hodgkin lymphoma were at increased risk for cancers of the esophagus, cecum, corpus uteri, and kidney; children with a first primary CNS were at increased risk for salivary gland tumors; children with a first primary bone tumor were at increased risk for cancers of the oral cavity and pharynx, respiratory system, and soft tissue; children with a first primary soft tissue tumor were at increased risk for kidney carcinoma and lymphatic and hematopoietic diseases; children with a first primary germ cell tumor were at increased risk for cancers of the CNS and lymphatic and hematopoietic diseases; and children with a first thyroid tumor were at increased risk for cancers of the salivary gland and kidney.
Further research regarding connections among these cancer types as well as further follow-up in this population are warranted in order to better understand subsequent cancer risk over the life span among childhood cancer survivors.
Competing Interests
The authors declare that they have no conflicts of interest.
Authors’ Contributions
RMM: Analyzed and described the data, assisted in the literature review, and wrote the paper.
AAS: Assisted in the literature review and writing the paper.
.
Authors’ Information
RMM: Professor of Cancer Epidemiology and Biostatistics at Brigham Young University. Former Visiting fellow at the International Agency for Research on Cancer in Lyon, France, and former fellow at the National Cancer Institute, Rockville, Maryland.
AAS: Student of Public Health at Brigham Young University.
Abbreviations
O = observed number of subsequent (2nd, 3rd, etc.) primary cancers; E = expected number of cancers in the general population; O/E = ratio of observed to expected cancers; CI: confidence interval; SEER: Surveillance, Epidemiology and End Results; CNS = central nervous system, including brain; Excess absolute risk (excess cancers per 10,000 person years, calculated as [(O-E)/person-years at risk] × 10,000).
Acknowledgements
We would like to thank Elizabeth Brutsch for her comments on the manuscript and suggestion of additional references.
References
[1]. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ.Cancer Statistics, 2008. CA Cancer J Clin. 2008, 58:71–96. [pubmed]
[2]. Inskip PD, Ries LAG, Cohen RJ, Curtis RE.New malignancies following childhood cancer. In New Malignancies among Cancer Survivors: SEER Cancer Registries, 1973-2000. National Cancer Institute. Edited by Curtis RE, Freedman DM, Ron E, Ries LAG, Hacker DG, Edwards BK, Tucker MA, Fraumeni JF Jr. (eds). NIH Publ. No. 05-5302. Bethesda, MD. 2006:465-482.
[3]. Ries LG, Smith MA, Gurney JG, et al (eds). Cancer Incidence and Survival among Children and Adolescents: United States SEER Program 1975-1995. NIH Pub. No. 99-4649. Bethesda, MD, National Cancer Institute; 1999.
[4]. Ries LG, Eisner MP, Kosary CL, et al (eds).SEER Cancer Statistics Review, 1975-2001. Bethesda, MD, National Cancer Institute, 2004.
[5]. Seer Cancer Statistics Review, 1975-2010 [Http://Seer.Cancer.Gov/Csr/1975_2010/].Bethesda: National Cancer Institute. 2010-13.
[6]. Kohler BA, Ward E, McCarthy BJ, Schymura MJ, Ries LA, Eheman C, Jemal A, Anderson RN, Ajani UA, Edwards BK.Annual report to the nation on the status of cancer, 1975-2007, featuring tumors of the brain and other nervous system. J Natl Cancer Inst.2011;103(9):14-36.[pubmed]
[7]. Meadows AT, Friedman DL, Neglia JP, Mertens AC, Donaldson SS, Stovall M, Hammond S, Yasui Y, Inskip PD. Second neoplasms in survivors of childhood cancer: findings from the Childhood Cancer Survivor Study cohort. J ClinOncol 2009;27:2356-2362[pubmed]
[8] Wendland MM, Tsodikov A, Glenn MJ, Gaffney DK.Time interval to the development of breast carcinoma after treatment for Hodgkin disease. Cancer 2004;101(6):1275-1282.[pubmed]
[9]. Cohen RJ, Curtis RE, Inskip PD, Fraumeni JF Jr.The risk of developing second cancers among survivors of childhood soft tissue sarcoma. Cancer 2005;103(11):2391-2396.[pubmed]
[10]. Reulen RC, Taylor AJ, Winter DL, Stiller CA, Frobisher C, Lancashire ER, McClanahan FM, Sugden EM, Hawkins MM. British ChildhoodCancer Survivor Study The British ChildhoodCancer Survivor Study (BCCSS) Steering Group: Long-term population-based risks of breast cancer after childhood cancer. Int J Cancer2008;123:2156-2163.
[11]. Hawkins MM, Lancashire ER, Winter DL, Frobisher C, Reulen RC, Taylor AJ, Stevens MC, Jenney M. The British Childhood Cancer Survivor Study: Objectives, methods, population structure, response rates and initial descriptive information. Pediatr Blood Cancer 2008;50(5):1018-1125.
[12]. Inskip PD, Curtis RE.New malignancies following childhood cancer in the United States, 1973-2002. Int J Cancer 2007:121(10):2233-2240.[pubmed]
[13]. Robison LL, Armstrong GT, Boice JD, Chow EJ, Davies SM, Donaldson SS, Green DM, Hammond S, Meadows AT, Mertens AC, Mulvihill JJ, Nathan PC, Neglia JP, Packer RJ, Rajaraman P, Sklar CA, Stovall M, Strong LC, Yasui Y, Zeltzer LK. The childhood cancer survivor study: a national cancer institute-supported resource for outcome and intervention research.J ClinOncol. 2009;27(14):2308-2318.[pubmed]
[14]. Surveillance Epidemiology and End Results.Documentation and recodes: International classification of childhood cancer [http://seer.cancer.gov/iccc/]. Washington: National Cancer Institute. 2011-13 [updated 2011; cited 2013 May 9].
[15]. Kramárová E, Stiller CA.The international classification of childhood cancer. Int J Cancer 1996;68(6):759-765.[pubmed]
[16]. Seer*Stat Database: Incidence [Http://Seer.Cancer.Gov]. Seer 9 Regs Research Data, Sub (1973-2010). 2010-13 [Updated Nov 2012; Cited 2013 May 14].
[17]. Neglia JP, Friedman DL, Yasui Y, Mertens AC, Hammond S, Stovall M, Donaldson SS, Meadows AT, Robison LL: Second malignant neoplasms in five-year survivors of childhood cancer: childhood cancer survivor study. J Natl Cancer Inst2011;93(8):618-629. [pubmed]
[18]. Reulen RC, Frobisher C, Winter DL, Kelly J, Lancashire ER, Stiller CA, Pritchard-Jones K, Jenkinson HC, Hawkins MM; British ChildhoodCancer Survivor Study Steering Group: Long-term risks of subsequent primary neoplasms among survivors of childhood cancer. JAMA2011;305(22):2311-2319.
[19]. Castellino SM, Geiger AM, Mertens AC, Leisenring WM, Tooze JA, Goodman P, Stovall M, Robison LL, Hudson MM. Morbidity and mortality in long-term survivors of Hodgkin lymphoma: a report from the childhood cancer survivor study. Blood 2011;117(6):1806-1816.[pubmed]
[20]. Maule M, Scélo G, Pastore G, Brennan P, Hemminki K, Olsen JH, Tracey E, Pukkala E, Weiderpass E, Brewster DH, Tamaro S, Chia KS, Pompe-Kirn V, Kliewer EV, Tonita JM, Martos C, Jonasson JG, Merletti F, Boffetta P.Second malignancies after childhood noncentral nervous system solid cancer: Results from 13 cancer registries. Intl J Cancer 2011;129(8):1940-1952.
[21]. Henderson TO, Whitton J, Stovall M, Mertens AC, Mitby P, Friedman D, Strong LC, Hammond S, Neglia JP, Meadows AT, Robison L, Diller LL.Secondary sarcomas in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst.2007;99:300-308. [pubmed]
[22]. Veiga LH, Bhatti P, Ronckers CM, Sigurdson AJ, Stovall M, Smith SA, Weathers R, Leisenring W, Mertens AC, Hammond S, Neglia JP, Meadows AT, Donaldson SS, Sklar CA, Friedman DL, Robison LL, Inskip PD.Chemotherapy and thyroid cancer risk: A report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev.2012;21(1):92-101.
[23]. Henderson TO, Rajaraman P, Stovall M, Constine LS, Olive A, Smith SA, Mertens A, Meadows A, Neglia JP, Hammond S, Whitton J, Inskip PD, Robison LL, Diller L.Risk factors associated with secondary sarcomas in childhood cancer survivors: a report from the childhood cancer survivor study. Intl J Rad Oncol, BiologyPhysics2012;84(1):224-230[pubmed]
[24]. Boukheris H, Stovall M, Gilbert ES, Stratton KL, Smith SA, Weathers R, Hammond S, Mertens AC, Donaldson SS, Armstrong GT, Robison LL, Neglia JP, Inskip PD: Risk of salivary gland cancer after childhood cancer: a report from the Childhood Cancer Survivor Study. Int J RadiatOncolBiol Phys. 2013;85(3):776-783[piubmed]
[25]. Nottage K, McFarlane J, Krasin MJ, Li C, Srivastava D, Robison LL, Hudson MM: Secondary colorectal carcinoma after childhood cancer. J ClinOncol. 2012;30(20):2552-2558.[pubmed]
[26]. Bowers DC, Nathan PC, Constine L, Woodman C, Bhatia S, Keller K, Bashore L:Subsequent neoplasms of the CNS among survivors of childhood cancer: A systematic review. Lancet Oncol. 2013;14(8):e321-328.[pubmed]
[27]. Bhatia S, Robison LL, Oberlin O, Greenberg M, Bunin G, Fossati-Bellani F, Meadows AT.Breast cancer and other second neoplasms after childhood Hodgkin’s disease. N Engl J Med 1996;334:745-751]pubmed]
[28]. Paulino AC, Fowler BZ. Secondary neoplasms after radiotherapy for a childhood solid tumor. PediatrHematolOncol 2005;22(2):89-101.[pubmed]
[29]. Carroll WL, Finlay J. Cancer in Children and Adolescents. Sudbury, MA: Jones and Bartlett; 2010.
[30]. Davies RP, Slavotinek JP, Dorney SFA. VIP secreting tumors in infancy. PediatrRadiol 1990;20(7):504-508. [pubmed]
[31]. Friedman DL, Whitton J, Leisenring W,Mertens AC, Hammond S, Stovall M, Donaldson SS, Meadows AT, Robison LL, Neglia JP.Subsequent neoplasms in 5-year survivors of childhood cancer: The childhood cancer survivor study. J Natl Cancer Inst 2010;102(14):1083-1095.[pubmed]
[32]. Gold DG, Neglia JP, Dusenbery KE. Second neoplasms after megavoltage radiation for pediatric tumors. Cancer2003;97(10):2588-2596. [pubmed]
[33]. Haddy TB, Mosher RB, Dinndorf PA, Reaman GH: Second neoplasms in survivors of childhood and adolescent cancer are often treatable. J Adolesc Health 2004;34(4):324-329. [pubmed]
[34]. Cardous-Ubbink MC, Heinen RC, Bakker PJM, van den Berg H, Oldenburger F, Caron HN, et al. Risk of second malignancies in long-term survivors of childhood cancer. Eur J Cancer. 2007;43:351-362. [pubmed]
[35]. Sklar CA, Mertens AC, Mitby P, Occhiogrosso G, Qin J, Heller G, Yasui Y, Robison LL: Risk of disease recurrence and second neoplasms in survivors of childhood cancer treated with growth hormone: a report from the childhood cancer survivor study. J ClinEndocrinolMetab.2002;87(7):3136-3141.[pubmed]
[36]. Van der Waal RIF, Veerman AJP, Snow GB, van der Waal I: Oral squamous cell carcinoma following treatment of acute lymphoblastic leukaemia. J Oral Pathol Med.1997;26:8-9[pubmed]
[37]. Chow EJ, Friedman DL, Stovall M, Yasui Y, Whitton JA, Robison LL, Sklar CA. Risk of thyroid dysfuncton and subsequent thyroid cancer among survivors of acute lymphoblastic leukemia: A report from the childhood cancer survivor study. Pediatr Blood Cancer 2009;53:432-437.
[38]. Brunetti D, Tamaro P, Fanin R, Cavallieri F, Stanta G.Family history of cancer and risk of second malignancies in young cancer patients in Trieste Italy. Int J Cancer 2005;115:814-821[pubmed]
[39]. Landmann E, Ochlies I, Zimmermann M, Moser O, Graf N, Suttorp M, Greiner J, Reiter A; Berlin-Frankfurt-Münster group. Secondary non-Hodgkin lymphoma (NHL) in children and adolescents after childhood cancer other than NHL. Br J Haematol. 2008;143:387-394[pubmed]
[40]. Pappo AS, Armstrong GT, Liu W, Srivastava DK, McDonald A, Leisenring WM, Hammond S, Stovall M, Neglia JP, Robison LL.Melanoma as a subsequent neoplasm in adult survivors of childhood cancer: A report from the childhood cancer survivor study. Pedr Blood & Cancer 2013;60:461-466[pubmed]
[41]. Neglia JP, Robison LL, Stovall M, Liu Y, Packer RJ, Hammond S, Yasui Y, Kasper CE, Mertens AC, Donaldson SS, Meadows AT, Inskip PD.New primary neoplasms of the central nervous system in survivors of childhood cancer. J Natl Cancer Inst 2006;98(21):1528-1537. [pubmed]
[42]. Yasui Y, Liu Y, Neglia JP, Friedman DL, Bhatia S, Meadows AT, Diller LR, Mertens AC, Whitton J, Robison LL.A methodological issue in the analysis of second-primary cancer incidence in long-term survivors of childhood cancers. Am J Epidemiol2003;158(11):1108-1113.[pubmed]
[43]. Davies SM.Subsequent malignant neoplasms in survivors of childhood cancer: Childhood Cancer Survivor Study (CCSS) studies. Pediatr Blood Cancer2007;48:727-730. [pubmed]
[44]. Kenney LB, Yasui Y, Inskip PD, Hammond S, Neglia JP, Mertens AC, Meadows AT, Friedman D, Robison LL, Diller L.Breast cancer in women who survived childhood cancer. Ann Intern Med. 2004;141:590-597[pubmed]
[45]. Travis LB, Hill D, Dores GM, Gospodarowicz M, van Leeuwen FE, Holowaty E, Glimelius B, Andersson M, Pukkala E, Lynch CF, Pee D, Smith SA, Van't Veer MB, Joensuu T, Storm H, Stovall M, Boice JD Jr, Gilbert E, Gail MH.Cumulative absolute breast cancer risk for young women treated for Hodgkin lymphoma. J Natl Cancer Inst. 2005;97(19):1428-1437[pubmed]
[46]. Hancock SL, Tucker MA, Hoppe, RT.Breast cancer after treatment of Hodgkin’s disease. J Natl Cancer Inst.1993;85(1):25-31[pubmed]
[47]. Nathan PC, Ness KK, Mahoney MC, Li Z, Hudson MM, Ford JS, Landier W, Stovall M, Armstrong GT, Henderson TO, Robison LL, Oeffinger KC.Screening and surveillance for second malignant neoplasms in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Ann Intern Med 2011;153(7):442-451[pubmed]
[48]. Jazbec J, Ecimovic P, Jereb B. Second neoplasms after treatment of childhood cancer in Slovenia. Pediatr Blood Cancer2004;42:574-581.[pubmed]
[49]. Tukenova M, Diallo I, Hawkins M, Guibout C, Quiniou E, Pacquement H, Dhermain F, Shamsaldin A, Oberlin O, de Vathaire F.Long-term mortality from second malignant neoplasms in 5-year survivors of solid childhood tumors: temporal pattern risk according to type of treatment. Cancer Epidemiol Biomarkers2010;19:707-715.
[50]. Guérin S, Dupuy A, Anderson H, Shamsaldin A, Svahn-Tapper G, Moller T, Quiniou E, Garwicz S, Hawkins M, Avril MF, Oberlin O, Chavaudra J, de Vathaire F.Radiation dose as a risk factor for malignant melanoma following childhood cancer. Eur J Cancer 2003, 39:2379-2386. [pubmed]
[51]. de Vathaire F, Hawkins M, Campbell S, Oberlin O, Raquin MA, Schlienger JY, Shamsaldin A, Diallo I, Bell J, Grimaud E, Hardiman C, Lagrange JL, Daly-Schveitzer N, Panis X, Zucker JM, Sancho-Garnier H, Eschwège F, Chavaudra J, Lemerle J.Second malignant neoplasms after a first cancer in childhood: temporal pattern of risk according to type of treatment. Br J Cancer 1999;79:1884-1893.
[52]. MacArthur AC, Spinelli JJ, Rogers PC, Goddard KJ, Phillips N, McBride ML.Risk of a second malignant neoplasm among 5-year survivors of cancer in childhood and adolescence in British Columbia, Canada. Pediatr Blood Cancer 2007;48:453-459.[pubmed]
[53]. Maule M, Scélo G, Pastore G, Brennan P, Hemminki K, Pukkala E, Weiderpass E, Olsen JH, Tracey E, McBride ML, Brewster DH, Pompe-Kirn V, Tonita JM, Kliewer EV, Chia KS, Jonasson JG, Martos C, Magnani C, Boffetta P.Risk of second malignant neoplasms after childhood central nervous system malignant tumours: An international study. Eur J Cancer 2008;44:830-839.
[54]. Garwicz S, Anderson H, Olsen JH, Døllner H, Hertz H, Jonmundsson G, Langmark F, Lanning M, Möller T, Sankila R, Tulinius H.Second malignant neoplasms after cancer in childhood and adolescence: a population-based case-control study in the 5 Nordic countries. Int J Cancer 2000;88:672-678[pubmed]
[55]. Haddy N, Le Deley MC, Samand A, Diallo I, Guérin S, Guibout C, Oberlin O, Hawkins M, Zucker JM, de Vathaire F.Role of radiotherapy and chemotherapy in the risk of secondary leukemia after a solid tumour in childhood. Eur J Cancer2006;42:2757-2764[pubmed]
[56]. Laverdière C, Liu Q, Yasui Y, Nathan PC, Gurney JG, Stovall M, Diller LR, Cheung NK, Wolden S, Robison LL, Sklar CA.Long-term outcomes in survivors of neuroblastoma. J Natl Cancer Inst2009;101:1131-1140[pubmed]
[57]. Rubino C, Adjadj E, Guérin S, Guibout C, Shamsaldin A, Dondon MG, Valteau-Couanet D, Hartmann O, Hawkins M, de Vathaire F.Long-term risk of second malignant neoplasms after neuroblastoma in childhood: role of treatment. Int J Cancer 2003;107:791-796[pubmed]
[58]. Bluhm EC, Ronckers C, Hayashi RJ, Neglia JP, Mertens AC, Stovall M, Meadows AT, Mitby PA, Whitton JA, Hammond S, Barker JD, Donaldson SS, Robison LL, Inskip PD: Cause-specific mortality and second cancer incidence after non-Hodgkin lymphoma: A report from the Childhood Cancer Survivor Study. Blood J2008;111:4014-4021.
[59]. Leung W, Sandlund JT, Hudson MM, Zhou Y, Hancock ML, Zhu Y, Ribeiro RC, Rubnitz JE, Kun LE, Razzouk B, Evans WE, Pui CH.Second malignancy after treatment of childhood non-Hodgkin lymphoma. Cancer 2001;92(7):1959-1966.[pubmed]
[60]. The Childhood Brain Tumor Foundation. Brain stem gliomas in childhood [http://www.childhoodbraintumor.org/index.php?view=article&catid=34%3Abrain-tumor types-and-imaging&id=57%3Abrain-stem-gliomasinchildhood&format=pdf&option=com_content&Itemid=53]. 2010-2013 [updated 2010; retrieved 2012 October 1].
[61]. Ceha HM, Balm AJ, de Jong D, van 't Veer LJ.Multiple malignancies in a patient with bilateral retinoblastoma.J Laryngol Otol. 1998;112(2):189-192.[pubmed]
[62]. Bhagia P, Colanta AB, Abramson DH, Carlson DL, Kleinerman RA, Kraus D, Dunkel IJ.Sinonasal adenocarcinoma: A rare second malignancy in long term retinoblastoma survivors.Pediatr Blood Cancer 2011;57(4):693-695[pubmed]
[63]. Bataille V, Hiles R, Bishop JA.Retinoblastoma, melanoma and the atypical mole syndrome. Br J Dermatol.1995;132(1):134-138[pubmed]
[64]. Wong FL, Boice JD Jr, Abramson DH, Tarone RE, Kleinerman RA, Stovall M, Goldman MB, Seddon JM, Tarbell N, Fraumeni JF Jr, Li FP.Cancer incidence after retinoblastoma. Radiation dose and sarcoma risk. JAMA 1997;278(15):1262-1267[pubmed]
[65]. NCI[http://www.cancer.gov/cancertopics/pdq/treatment/thyroid/Patient/page4]. Treatment option overview. Washington: National Cancer Institute; 2013 [updated 2013 January 11; cited 2013 May 11].
[66]. MD Anderson Cancer Center. Childhood melanoma[http://www.mdanderson.org/pati nt-and-cancer-information/cancer information/cancer-types/childhood-melanoma/index.html].
[67]. Vezzadini C, Cremonini N, Sforza A, Presutti L, Chiarini V.Treated Wilm's tumor in childhood as potential risk factor for second thyroid cancer.Panminerva Med 2002;44(3):275-277.[pubmed]
[68]. NCI[http://seer.cancer.gov/archive/csr/1975_2003/results_single/sect_01_table.11_2pgs.pdf]. Median age of cancer patients at diagnosis. [n.d.].

